Amoebiasis
Amoebiasis, or amoebic dysentery, is an infection of the intestines caused by a parasitic amoeba Entamoeba histolytica.
[2] Diagnosis is made by stool examination using microscopy, but it can be difficult to distinguish E. hystolitica from other harmless entamoeba species.
Extra-intestinal complications might also arise as a result of invasive infection which includes colitis, liver, lung, or brain abscesses.
[citation needed] Onset time is highly variable and the average asymptomatic infection persists for over a year.
It is theorized that the absence of symptoms or their intensity may vary with such factors as strain of amoeba, immune response of the host, and perhaps associated bacteria and viruses.
[citation needed] In asymptomatic infections, the amoeba lives by eating and digesting bacteria and food particles in the gut, a part of the gastrointestinal tract.
Especially in Latin America,[citation needed] a granulomatous mass (known as an amoeboma) may form in the wall of the ascending colon or rectum due to long-lasting immunological cellular response, and is sometimes confused with cancer.
[12] Steroid therapy can occasionally provoke severe amoebic colitis in people with any E. histolytica infection.
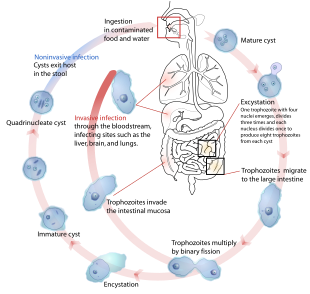
Infection is spread through ingestion of the cyst form of the parasite, a semi-dormant and hardy structure found in feces.
Any non-encysted amoebae, or trophozoites, die quickly after leaving the body but may also be present in stool: these are rarely the source of new infections.
[9] Since amoebiasis is transmitted through contaminated food and water, it is often endemic in regions of the world with limited modern sanitation systems, including México, Central America, western South America, South Asia, and western and southern Africa.
E. histolytica causes tissue damage by three main events: direct host cell killing, inflammation, and parasite invasion.
[16] The pathogenesis of amoebiasis involves interplay of various molecules secreted by E. histolytica such as LPPG, lectins, cysteine proteases, and amoebapores.
[17] With colonoscopy it is possible to detect small ulcers of between 3–5mm, but diagnosis may be difficult as the mucous membrane between these areas can look either healthy or inflamed.
[2] Trophozoites may be identified at the ulcer edge or within the tissue, using immunohistochemical staining with specific anti-E. histolytica antibodies.
Since antibodies may persist for years after clinical cure, a positive serological result may not necessarily indicate an active infection.
E.histolytica cysts are usually resistant to chlorination, therefore sedimentation and filtration of water supplies are necessary to reduce the incidence of infection.
(Mistaken for Ca caecum and appendicular mass) Other local complications include bloody diarrhea, pericolic and pericaecal abscess.
[citation needed] Pulmonary amoebiasis can occur from liver lesions by spread through the blood or by perforation of pleural cavity and lung.
[citation needed] Nevertheless, this means that there are up to 50 million true E. histolytica infections and approximately seventy thousand die each year, mostly from liver abscesses or other complications.
Although usually considered a tropical parasite, the first case reported (in 1875) was actually in St Petersburg in Russia, near the Arctic Circle.
[23] Infection is more common in warmer areas, but this is because of both poorer hygiene and the parasitic cysts surviving longer in warm moist conditions.
[2][9] The most dramatic incident in the US was the Chicago World's Fair outbreak in 1933, caused by contaminated drinking water.
[2] Joel Connolly of the Chicago Bureau of Sanitary Engineering brought the outbreak to an end when he found that defective plumbing permitted sewage to contaminate drinking water.
[citation needed] The Nicobarese people have attested to the medicinal properties found in Glochidion calocarpum, a plant common to India, saying that its bark and seed are most effective in curing abdominal disorders associated with amoebiasis.