Anthrax
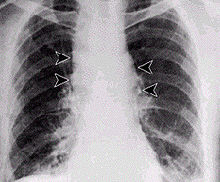
[27] These symptoms may be accompanied by cough, shortness of breath, chest pain, and nausea or vomiting, making inhalation anthrax difficult to distinguish from influenza and community-acquired pneumonia.
[28] Gastrointestinal (GI) infection is most often caused by consuming anthrax-infected meat and is characterized by diarrhea, potentially with blood, abdominal pains, acute inflammation of the intestinal tract, and loss of appetite.
Once ingested or placed in an open wound, the bacteria begin multiplying inside the animal or human and typically kill the host within a few days or weeks.
The spores are then picked up by scavenger cells (macrophages) in the lungs and transported through small vessels (lymphatics) to the lymph nodes in the central chest cavity (mediastinum).
Anthrax can enter the human body through the intestines (gastrointestinal), lungs (pulmonary), or skin (cutaneous), and causes distinct clinical symptoms based on its site of entry.
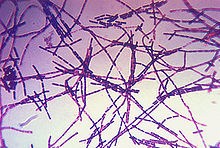
B. anthracis colonies are medium-large, gray, flat, and irregular with swirling projections, often referred to as having a "medusa head" appearance, and are not hemolytic on 5% sheep blood agar.
All currently used anthrax vaccines show considerable local and general reactogenicity (erythema, induration, soreness, fever) and serious adverse reactions occur in about 1% of recipients.
[55] The American product, BioThrax, is licensed by the FDA and was formerly administered in a six-dose primary series at 0, 2, 4 weeks and 6, 12, 18 months, with annual boosters to maintain immunity.
In response to the anthrax attacks of October 2001, the United States Postal Service (USPS) installed biodetection systems (BDSs) in their large-scale mail processing facilities.
[62] In May 2009, Human Genome Sciences submitted a biologic license application (BLA, permission to market) for its new drug, raxibacumab (brand name ABthrax) intended for emergency treatment of inhaled anthrax.
Legler, et al.[66] showed that pegylated CapD (capsule depolymerase) could provide protection against 5 LD50 exposures to lethal Ames spores without the use of antibiotics, monoclonal antibodies, or vaccines.
[8] The last fatal case of natural inhalational anthrax in the United States occurred in California in 1976, when a home weaver died after working with infected wool imported from Pakistan.
The case involved a maker of traditional African-style drums who was working with a goat hide purchased from a dealer in New York City which had been previously cleared by Customs.
[78] In July 2022, dozens of cattle in a nature park in Lonjsko Polje, a flood plain by the Sava river, died of anthrax and 6 people have been hospitalized with light, skin-related symptoms.
John Henry Bell, a doctor born & based in Bradford, first made the link between the mysterious and deadly "woolsorter's disease" and anthrax, showing in 1878 that they were one and the same.
[83] In the early 20th century, Friederich Wilhelm Eurich, the German bacteriologist who settled in Bradford with his family as a child, carried out important research for the local Anthrax Investigation Board.
Eurich also made valuable contributions to a Home Office Departmental Committee of Inquiry, established in 1913 to address the continuing problem of industrial anthrax.
French scientist Louis Pasteur was charged with the production of a vaccine, following his successful work in developing methods that helped to protect the important wine and silk industries.
[85] In May 1881, Pasteur – in collaboration with his assistants Jean-Joseph Henri Toussaint, Émile Roux and others – performed a public experiment at Pouilly-le-Fort to demonstrate his concept of vaccination.
He used his celebrity status to establish Pasteur Institutes across Europe and Asia, and his nephew, Adrien Loir, travelled to Australia in 1888 to try to introduce the vaccine to combat anthrax in New South Wales.
To speed the process, trace amounts of a nontoxic catalyst composed of iron and tetroamido macrocyclic ligands are combined with sodium carbonate and bicarbonate and converted into a spray.
Its first modern incidence occurred when Nordic rebels, supplied by the German General Staff, used anthrax with unknown results against the Imperial Russian Army in Finland in 1916.
Ultimately, five million pellets were created, though plans to drop them over Germany using Royal Air Force bombers in 1944 were scrapped after the success of Operation Overlord and the subsequent Allied liberation of France.
[111] American military and British Army personnel are no longer routinely vaccinated against anthrax prior to active service in places where biological attacks are considered a threat.
On 2 April 1979, some of the over one million people living in Sverdlovsk (now called Ekaterinburg, Russia), about 1,370 kilometres (850 mi) east of Moscow, were exposed to an accidental release of anthrax from a biological weapons complex located near there.
[116] In addition to the medical problems the outbreak caused, it also prompted Western countries to be more suspicious of a covert Soviet bioweapons program and to increase their surveillance of suspected sites.
[118] To make large amounts of an aerosol form of anthrax suitable for biological warfare requires extensive practical knowledge, training, and highly advanced equipment.
[35] Only a few grams of material were used in these attacks and in August 2008, the US Department of Justice announced they believed that Bruce Ivins, a senior biodefense researcher employed by the United States government, was responsible.
Due to these events, the US Postal Service installed biohazard detection systems at its major distribution centers to actively scan for anthrax being transported through the mail.
[124] A scientific experiment performed by a high school student, later published in the Journal of Medical Toxicology, suggested a domestic electric iron at its hottest setting (at least 400 °F (204 °C)) used for at least 5 minutes should destroy all anthrax spores in a common postal envelope.