Artificial heart valve
[citation needed] Companies that manufacture heart valves include Edwards Lifesciences,[5] Medtronic,[6] Abbott (St. Jude Medical),[7] CryoLife,[8] and LifeNet Health.
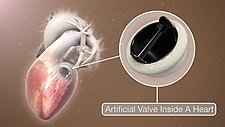
[9] Mechanical valves come in three main types – caged ball, tilting-disc and bileaflet – with various modifications on these designs.
When the heart finishes contracting, the pressure inside the chamber drops and the ball moves back against the base of the valve forming a seal.
[13] Caged ball valves are strongly associated with blood clot formation, so people who have one required a high degree of anticoagulation, usually with a target INR of 3.0–4.5.
With a larger opening than caged ball or tilting-disc valves, they carry a lower risk of blood clots.
People with mechanical valves need to take anticoagulants (blood thinners), such as warfarin, for the rest of their life.
[citation needed] Cavitation, the rapid formation of microbubbles in a fluid such as blood due to a localized drop of pressure, can lead to mechanical heart valve failure,[17] so cavitation testing is an essential part of the valve design verification process.
For example, blood clot formation is a side effect of high shear stresses created by the design of the valves.
From an engineering perspective, an ideal heart valve would produce minimal pressure drops, have small regurgitation volumes, minimize turbulence, reduce prevalence of high stresses, and not create flow separations in the vicinity of the valve.
[18][non-primary source needed] Bioprosthetic valves are usually made from animal tissue (heterograft/xenograft) attached to a metal or polymer support.
This procedure was first performed in 1967 and is used primarily in children, as it allows the patient's own pulmonary valve (now in the aortic position) to grow with the child.
[21] In recent years, scientists have developed a new tissue preservation technology, with the aim of improving the durability of bioprosthetic valves.
[23][non-primary source needed] Current bioprosthetic valves lack longevity, and will calcify over time.
[26] The scaffold acts as an extracellular matrix, guiding tissue growth into the correct 3D structure of the heart valve.
Tissue engineered heart valves can be person-specific and 3D modeled to fit an individual recipient[27] 3D printing is used because of its high accuracy and precision of dealing with different biomaterials.
[27] Cells that are used for tissue engineered heart valves are expected to secrete the extracellular matrix (ECM).
Due to the risk of forming blood clots for mechanical valves and severe bleeding as a major side effect of taking blood-thinning medications, people who have a risk of blood bleeding and are not willing to take warfarin may also consider tissue valves.
Other patients who may be more suitable for tissue valves are people who have other planned surgeries and unable to take blood-thinning medications.
[24] Researchers are investigating catheter-based surgery that allows repair of an artificial heart valve without large incisions.