Aspiration pneumonia
[2] Risk factors include decreased level of consciousness, problems with swallowing, alcoholism, tube feeding, and poor oral health.
[2] Signs and symptoms of aspiration pneumonia may develop gradually, with increased respiratory rate, foul-smelling sputum, hemoptysis, and fever.
[6] If continual aspiration occurs, the chronic inflammation can cause compensatory thickening of the insides of the lungs, resulting in bronchiectasis.
[14] They make up the majority of normal oral flora and the presence of putrid fluid in the lungs is highly suggestive of aspiration pneumonia secondary to an anaerobic organism.
[14] Potential anaerobic bacteria are as follows: Aspiration is defined as inhalation of oropharyngeal or gastric contents into the pulmonary tree.
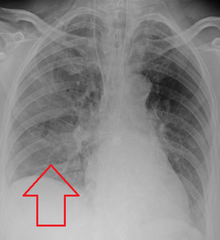
Generally, the right middle and lower lung lobes are the most common sites affected, due to the larger caliber and more vertical orientation of the right mainstem bronchus.
The right upper lobe is a common area of consolidation, where liquids accumulate in a particular region of the lung, in alcoholics who aspirate in the supine position.
[6] Likewise, physical exam findings such as altered breath sounds heard in the affected lung fields may also be suggestive of aspiration pneumonia.
[20] While aspiration pneumonia and chemical pneumonitis may appear similar, it is important to differentiate between the two due to major differences in management of these conditions.
[19] However, it is important to note that the findings of chemical pneumonitis are triggered by inflammation not caused by infection, as seen in aspiration pneumonia.
Thus, treatment of chemical pneumonitis typically involves removal of the inflammatory fluid and supportive measures, notably excluding antibiotics.
Certain risk factors predispose individuals to aspiration, especially conditions causing dysfunction of the upper gastrointestinal system.
[24] Other practices that may be beneficial but have not been well-studied include medication that reduce the acidity of gastric contents and rapid sequence induction.
It's crucial to keep a close eye on the patient's oxygen saturation, and if hypoxia is detected, urgent intubation with mechanical breathing should be given.
Flexible bronchoscopy is often used to gather samples of bronchoalveolar lavage for quantitative bacteriological tests as well as high volume aspiration to clear the secretion.
[25] In general practice The main treatment of aspiration pneumonia revolves around the use of antibiotics to remove the bacteria causing the infection.
[1] Broad antibiotic coverage is required to account for the diverse types of bacteria possibly causing the infection.
[28] Owing to multiple factors, such as frailty, impaired efficacy of swallowing, decreased cough reflex and neurological complications, dysphagia can be considered as a geriatric syndrome.
Aspiration pneumonia most often develops due to micro-aspiration of saliva, or bacteria carried on food and liquids, in combination with impaired host immune function.
[30] Chronic inflammation of the lungs is a key feature in aspiration pneumonia in elderly nursing home residents and presents as a sporadic fever (one day per week for several months).
[30] The reported prevalence of dysphagia in patients with Parkinson's disease ranges from 20% to 100% due to variations in the methods of assessing the swallowing function.
The familiar model of care for people with advanced dementia and dysphagia is the revolving door of recurrent chest infections, frequently associated with aspiration and related readmissions.