Mandibular fracture
[4] By far, the two most common symptoms described are pain and the feeling that teeth no longer correctly meet (traumatic malocclusion, or disocclusion).
For fractures that occur in the non-tooth bearing area (condyle, ramus, and sometimes the angle) an open bite is an important clinical feature since little else, other than swelling, may be apparent.
[5]: page number needed This type of fractured mandible can involve one condyle (unilateral) or both (bilateral).
[6] Bilateral body or parasymphysis fractures are sometimes termed "flail mandible", and can cause involuntary posterior movement of the tongue with subsequent obstruction of the upper airway.
[8] Other rare complications of mandibular trauma include internal carotid artery injury,[9] and obliteration of the ear canal due to posterior condylar dislocation.
[citation needed] Traditionally, plain films of the mandible would be exposed but had lower sensitivity and specificity owing to overlap of structures.
Because the curve of the mandible appears in a 2-dimensional image, fractures are easier to spot leading to an accuracy similar to CT except in the condyle region.
In addition, broken, missing or malaligned teeth can often be appreciated on a panoramic image which is frequently lost in plain films.
3D reconstruction, however, can mask smaller fractures owing to volume averaging, scatter artifact and surrounding structures simply blocking the view of underlying areas.
[citation needed] Research has shown that panoramic radiography is similar to computed tomography in its diagnostic accuracy for mandible fractures and both are more accurate than plain film radiograph.
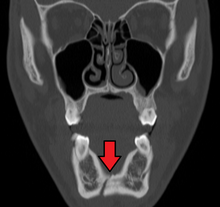
Condylar fractures are classified by location compared to the capsule of ligaments that hold the temporomandibular joint (intracapsular or extracapsular), dislocation (whether or not the condylar head has come out of the socket (glenoid fossa) as the muscles (lateral pterygoid) tend to pull the condyle anterior and medial) and neck of the condyle fractures.
[15] Because the coronoid process of the mandible lies deep to many structures, including the zygomatic complex (ZMC), it is rare to be broken in isolation.
When a fracture occurs in the tooth bearing portion of the mandible, whether or not it is dentate or edentulous will affect treatment.
When an edentulous mandible (no teeth) is less than 1 cm in height (as measured on panoramic radiograph or CT scan) additional risks apply because the blood flow from the marrow (endosseous) is minimal and the healing bone must rely on blood supply from the periosteum surrounding the bone.
[23][non-primary source needed] While mandible fractures have similar complication rates whether treated immediately or days later, older fractures are believed to have higher non-union and infection rates although the data on this makes it difficult to draw firm conclusions.
Except in avulsive type injuries, or those where there might be airway compromise, a several day delay in the treatment of mandible fractures seems to have little impact on the outcome or complication rates.
While rare, bilateral mandible fractures that are unstable can cause the tongue to fall back and block the airway.
Fractures such as a symphyseal or bilateral parasymphyseal may lead to mobility of the central portion of the mandible where genioglossus attaches, and allow the tongue to fall backwards and block the airway.
Loss of consciousness combined with aspiration of tooth fragments, blood and possibly dentures mean that the airway may be threatened.
Closed reduction may involve intermaxillary fixation, where the jaws are splinted together in the correct position for a period of weeks.
A systematic review was unable to find sufficient evidence of the superiority of one method over another in the management of condylar fractures.
[27] Paediatric condylar fractures are especially problematic, owing to the remaining growth potential and possibility of ankylosis of the joint.
In these cases, oral surgeons sometimes opt for external fixation, closed reduction, supraperiosteal dissection or other techniques to maintain the periosteal blood flow.
[30] In high velocity injuries, the soft tissue can be severely damaged far from the bullet wound itself due to hydrostatic shock.
[33] The healing time for a routine mandible fractures is 4–6 weeks whether MMF or rigid internal fixation (RIF) is used.
When the fracture is intracapsular there is a higher rate of late-term osteoarthritis and the potential for ankylosis although the later is a rare complication as long as mobilization is early.
[39] Prior to the routine use of seat belts, airbags and modern safety measures, motor vehicle collisions were a leading cause of facial trauma.
[40] With respect to trauma patients, roughly 10% have some sort of facial fracture, the majority of which come from motor vehicle collisions.
in the Edwin Smith Papyrus and later by Hippocrates in 460 B.C., "Displaced but incomplete fractures of the mandible where continuity of the bone is preserved should be reduced by pressing the lingual surface with the fingers...".
[42] Since the late 19th century, modern techniques including MMF (see above) have been described with titanium based rigid internal fixation becoming commonplace since the 1970s and biodegradable plates and screws being available since the 1980s.