Chorioamnionitis
[1] In 2015, a National Institute of Child Health and Human Development Workshop expert panel recommended use of the term "triple I" to address the heterogeneity of this disorder.
[2] Chorioamnionitis results from an infection caused by bacteria ascending from the vagina into the uterus and is associated with premature or prolonged labor.
[4] The risk of developing chorioamnionitis increases with number of vaginal examinations performed in the final month of pregnancy, including labor.
[11] Birthing-related events, lifestyle, and ethnic background have been linked to an increase in the risk of developing chorioamnionitis apart from bacterial causation.
[11] Premature deliveries, ruptures of the amniotic sac membranes, prolonged labor, and primigravida childbirth are associated with this condition.
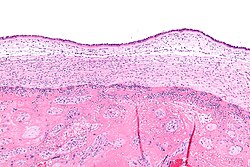
Diagnosis can be confirmed histologically or through amniotic fluid tests such as gram staining, glucose levels, or other culture results consistent with infection.
[9] In addition, it has been shown that it is not necessary to deliver the fetus quickly after chorioamnionitis is diagnosed, so a C-section is not necessary unless maternal health concern is present.
[12] However, research has found that beginning labor early at approximately 34 weeks can lessen the likelihood of fetal death, and reduce the potential for excessive infection within the mother.
[8] The American College of Obstetricians and Gynecologists' Committee Opinion proposes the use of antibiotic treatment in intrapartum mothers with suspected or confirmed chorioamnionitis and maternal fever without an identifiable cause.
Long-term infant complications like bronchopulmonary dysplasia, cerebral palsy, and Wilson-Mikity syndrome have been associated to the bacterial infection.
[19] For mother and fetus, chorioamnionitis may lead to short-term and long-term issues when microbes move to different areas or trigger inflammatory responses due to infection.
Disability development is related to the activation of the fetal inflammatory response syndrome (FIRS) when the fetus is exposed to infected amniotic fluid or other foreign entities.
Some studies have shown that the risk of chorioamnionitis is higher in those of African American ethnicity, those with immunosuppression, and those who smoke, use alcohol, or abuse drugs.