Decompression theory
In all cases, the symptoms caused by decompression occur during or within a relatively short period of hours, or occasionally days, after a significant pressure reduction.
The development of schedules that are both safe and efficient has been complicated by the large number of variables and uncertainties, including personal variation in response under varying environmental conditions and workload.
Under equilibrium conditions, the total concentration of dissolved gases will be less than the ambient pressure, as oxygen is metabolised in the tissues, and the carbon dioxide produced is much more soluble.
[7] Decompression involves a complex interaction of gas solubility, partial pressures and concentration gradients, diffusion, bulk transport and bubble mechanics in living tissues.
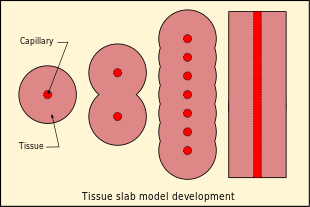
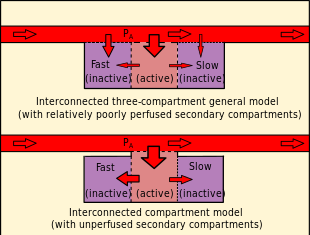
[7] The inert gases from the breathing gas in the lungs diffuse into blood in the alveolar capillaries and are distributed around the body by the systemic circulation in the process known as perfusion.
[32] Decompression bubbles appear to form mostly in the systemic capillaries where the gas concentration is highest, often those feeding the veins draining the active limbs.
The bubbles carried back to the heart in the veins may be transferred to the systemic circulation via a patent foramen ovale in divers with this septal defect, after which there is a risk of occlusion of capillaries in whichever part of the body they end up in.
[40] They suggest that breathing-gas switches from helium-rich to nitrogen-rich mixtures should be carefully scheduled either deep (with due consideration to nitrogen narcosis) or shallow to avoid the period of maximum supersaturation resulting from the decompression.
Although it is commonly held that DCS is caused by inert gas supersaturation, Hempleman has stated: ...This did not lead to a sufficient cut-back in the permitted decompression ratio and an allowance in the calculations is now made for high oxygen partial pressures.
For example, the most common inert gas diluent substitute for nitrogen is helium, which is significantly less soluble in living tissue,[47] but also diffuses faster due to the relatively small size and mass of the He atom in comparison with the N2 molecule.
[56] These have been attributed to the development of a relatively high gas phase volume which may be partly carried over to subsequent dives or the final ascent of a sawtooth profile.
[25] A number of empirical modifications to dissolved phase models have been made since the identification of venous bubbles by Doppler measurement in asymptomatic divers soon after surfacing.
This approach seeks to maximise the concentration gradient providing there are no symptoms, and commonly uses a slightly modified exponential half-time model.
The gradient factor is a percentage of the M-value chosen by the algorithm designer, and varies linearly between the maximum depth of the specific dive and the surface.
[69] Several models of dive computer allow user input of gradient factors as a way of inducing a more conservative, and therefore presumed lower risk, decompression profile.
[75] Forcing a low gradient factor at the deep M-value can have the effect of increasing ingassing during the ascent, generally of the slower tissues, which must then release a larger gas load at shallower depths.
(the shallow M-value is linked to actual depth of zero in both cases) [78] According to the thermodynamic model of Hugh LeMessurier and Brian Andrew Hills, this condition of optimum driving force for outgassing is satisfied when the ambient pressure is just sufficient to prevent phase separation (bubble formation).
[70] The critical-volume criterion assumes that whenever the total volume of gas phase accumulated in the tissues exceeds a critical value, signs or symptoms of DCS will appear.
The usefulness of the model is judged on its accuracy and reliability in predicting the onset of symptomatic decompression sickness and asymptomatic venous bubbles during ascent.
Their analysis strongly suggested that bubble presence limits gas elimination rates, and emphasized the importance of inherent unsaturation of tissues due to metabolic processing of oxygen.
The "deepest possible decompression stop" for a given profile can be defined as the depth where the gas loading for the leading compartment crosses the ambient pressure line.
[99] A study by DAN in 2004 found that the incidence of high-grade bubbles could be reduced to zero providing the nitrogen concentration of the most saturated tissue was kept below 80 percent of the allowed M value and that an added deep stop was a simple and practical way of doing this, while retaining the original ascent rate.
It is a long process during which inert gases are eliminated at a very low rate limited by the slowest affected tissues, and a deviation can cause the formation of gas bubbles which can produce decompression sickness.
Most operational procedures rely on experimentally derived parameters describing a continuous slow decompression rate, which may depend on depth and gas mixture.
A widespread belief developed that algorithms based on bubble models and which distribute decompression stops over a greater range of depths are more efficient than the traditional dissolved gas content models by minimising early bubble formation, based on theoretical considerations, largely in the absence of evidence of effectiveness, though there were low incidences of symptomatic decompression sickness.
It is well established both in theory and practice, that a higher oxygen partial pressure facilitates a more rapid and effective elimination of inert gas, both in the dissolved state and as bubbles.
This risk can be reduced by sufficient initial decompression, using high oxygen partial pressure and making the helium to nitrogen switch relatively shallow.
The dives and PFSI were followed by a four-hour exposure at 75 kPa, equivalent to the maximum permitted commercial aircraft cabin altitude of 8,000 feet (2,400 m).
[121] In-flight transthoracic echocardiography has shown that there is a low but non-zero probability of decompression sickness in commercial pressurised aircraft after a 24 hour pre-flight surface interval following a week of multiple repetitive recreational dives, indicated by detection of venous gas bubbles in a significant number of the divers tested.
For behind the "black-and-white" exactness of table entries, the second-by-second countdowns of dive computers, and beneath the mathematical purity of decompression models, lurks a dark and mysterious physiological jungle that has barely been explored.