Dialectical behavior therapy
Dialectical behavior therapy (DBT) is an evidence-based[1] psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts.
[1] Evidence suggests that DBT can be useful in treating mood disorders and suicidal ideation as well as for changing behavioral patterns such as self-harm and substance use.
[4] DBT grew out of a series of failed attempts to apply the standard cognitive behavioral therapy (CBT) protocols of the late 1970s to chronically suicidal clients.
[8][3] Research indicates that DBT might help patients with symptoms and behaviors associated with spectrum mood disorders, including self-injury.
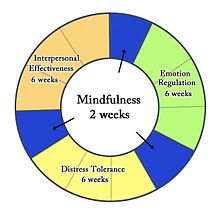
[11] DBT combines standard cognitive-behavioral techniques for emotion regulation and reality-testing with concepts of distress tolerance, acceptance, and mindful awareness largely derived from contemplative meditative practice.
DBT is based upon the biosocial theory of mental illness and is the first therapy that has been experimentally demonstrated to be generally effective in treating borderline personality disorder (BPD).
[14] DBT may not be appropriate as a universal intervention, as it was shown to be harmful or have null effects in a study of an adapted DBT skills-training intervention in adolescents in schools, though conclusions of iatrogenic harm are unwarranted as the majority of participants did not significantly engage with the assigned activities with higher engagement predicting more positive outcomes.
[19] DBT focuses on the client acquiring new skills and changing their behaviors,[20] with the ultimate goal of achieving a "life worth living".
[1] In DBT's biosocial theory of BPD, clients have a biological predisposition for emotional dysregulation, and their social environment validates maladaptive behavior.
It is considered a foundation for the other skills taught in DBT, because it helps individuals accept and tolerate the powerful emotions they may feel when challenging their habits or exposing themselves to upsetting situations.
The practice of mindfulness can also be intended to make people more aware of their environments through their five senses: touch, smell, sight, taste, and sound.
DBT has five specific states of change which the therapist will review with the patient: pre-contemplation, contemplation, preparation, action, and maintenance.
[27] The concept of distress tolerance arose from methods used in person-centered, psychodynamic, psychoanalytic, gestalt, and/or narrative therapies, along with religious and spiritual practices.
This allows individuals to make wise decisions about whether and how to take action, rather than falling into intense, desperate, and often destructive emotional reactions.
[38] The American Psychiatric Association (APA) does not recognize CPTSD as a diagnosis in the DSM-5 (Diagnostical and Statistical Manual of Mental Disorders, the manual used by providers to diagnose, treat and discuss mental illness), though many practitioners argue that CPTSD is separate from post-traumatic stress disorder (PTSD).
Different versions are contributed by the World Health Organization (WHO), The International Society for Traumatic Stress Studies (ISTSS), and individual clinicians and researchers.
In addition to affect dysregulation, case studies reveal that patients with CPTSD can also exhibit splitting, mood swings, and fears of abandonment.
[44][better source needed] Thus, treatment for CPTSD involves stabilizing and teaching successful coping behaviors, affect regulation, and creating and maintaining interpersonal connections.
DBT's use of acceptance and goal orientation as an approach to behavior change can help to instill empowerment and engage individuals in the therapeutic process.
Further, this argument posits that DBT decreases self-injurious behaviors (such as cutting or burning) and increases interpersonal functioning but neglects core CPTSD symptoms such as impulsivity, cognitive schemas (repetitive, negative thoughts), and emotions such as guilt and shame.
[38] Because DBT has four modules which generally align with these guidelines (Mindfulness, Distress Tolerance, Affect Regulation, Interpersonal Skills) it is a treatment option.
[48] A study co-authored by Linehan found that among women receiving outpatient care for BPD and who had attempted suicide in the previous year, 56% additionally met criteria for PTSD.
[49] Because of the correlation between borderline personality disorder traits and trauma, some settings began using DBT as a treatment for traumatic symptoms.
[50] Some providers opt to combine DBT with other PTSD interventions, such as prolonged exposure therapy (PE) (repeated, detailed description of the trauma in a psychotherapy session)[51] or cognitive processing therapy (CPT) (psychotherapy which addresses cognitive schemas related to traumatic memories).
[55] The first three modules of DBT increase distress tolerance and emotion regulation skills in the individual, paving the way for work on symptoms such as intrusions, self-esteem deficiency, and interpersonal relations.
For example, in veteran populations DBT is modified to include exposure exercises and accommodate the presence of traumatic brain injury (TBI), and insurance coverage (i.e. shortening treatment).