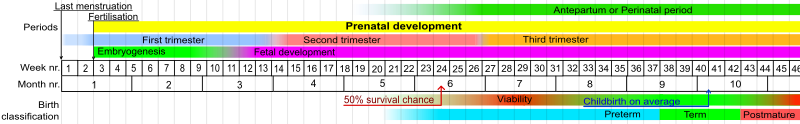
Fetal viability
[5] Viability, as the word has been used in the United States constitutional law since Roe v. Wade, is the potential of the fetus to survive outside the uterus after birth, natural or induced, when supported by up-to-date medicine.
[6] According to Websters Encyclopedic Unabridged Dictionary of the English Language, viability of a fetus means having reached such a stage of development as to be capable of living, under normal conditions, outside the uterus.
It is the antithesis of viable, which is defined as having attained such form and development of organs as to be normally capable of living outside the uterus."
That stage of fetal development when the life of the unborn child may be continued indefinitely outside the womb by natural or artificial life-support systems.
For purposes of abortion regulation, viability is reached when, in the judgement of the attending physician on the particular facts of the case before him or her, there is a reasonable likelihood of the fetuses' sustained survival outside the womb, with or without artificial support.
[16] Prognosis depends also on medical protocols on whether to resuscitate and aggressively treat a very premature newborn, or whether to provide only palliative care, in view of the high risk of severe disability of very preterm babies.
Medical decisions regarding the resuscitation of extremely preterm infants (EPI) deemed to be in the "grey zone" usually take into account weight and gestational age, as well as parental views.
[26] The subsequent Planned Parenthood v. Casey (1992) modified the "trimester framework", permitting the states to regulate abortion in ways not posing an "undue burden" on the right of the mother to an abortion at any point before viability; on account of technological developments between 1973 and 1992, viability itself was legally dissociated from the hard line of 28 weeks, leaving the point at which "undue burdens" were permissible variable depending on the technology of the time and the judgement of the state legislatures.
It defines "born alive" as "the complete expulsion or extraction from his or her mother of that member, at any stage of development, who after such expulsion or extraction breathes or has a beating heart, pulsation of the umbilical cord, or definite movement of voluntary muscles"[27] and specifies that any of these is the action of a living human person.
While the implications of this law for defining viability in medicine may not be fully explored,[28] in practice doctors and nurses are advised not to resuscitate such persons with gestational age of 22 weeks or less, under 400 g weight, with anencephaly, or with a confirmed diagnosis of trisomy 13 or 18.
[29][30] Forty-three states have laws banning post-viability abortions unless pregnancy threatens the life or health of the woman or there is a fetal abnormality.
The procedure intact dilation and extraction (IDX) became a focal point in the abortion debate,[31] based on the belief that it is used mainly post-viability.
[32] IDX was made illegal in most circumstances by the Partial-Birth Abortion Ban Act in 2003, which the U.S. Supreme Court upheld in the case of Gonzales v. Carhart.
For example, breathing problems, congenital abnormalities or malformations, and the presence of other severe diseases, especially infection, threaten the survival of the neonate.
[citation needed] Other factors may influence survival by altering the rate of organ maturation or by changing the supply of oxygen to the developing fetus.
[16] The quality of the facility—whether the hospital offers neonatal critical care services, whether it is a Level I pediatric trauma care facility, the availability of corticosteroids and other medications at the facility, the experience and number of physicians and nurses in neonatology and obstetrics and of the providers has a limited but still significant impact on fetal viability.