Frostbite
[2][1] People who are exposed to low temperatures for prolonged periods, such as winter sports enthusiasts, military personnel, and homeless individuals, are at greatest risk.
[7][1] Other risk factors include drinking alcohol, smoking, mental health problems, certain medications, and prior injuries due to cold.
[2][1] Rapid heating or cooling should be avoided since it could potentially cause burning or heart stress.
[9] Rubbing or applying force to the affected areas should be avoided as it may cause further damage such as abrasions.
[2] The use of ibuprofen and tetanus toxoid is recommended for pain relief or to reduce swelling or inflammation.
[1] The first formal description of the condition was in 1813 by Dominique Jean Larrey, a physician in Napoleon's army, during its invasion of Russia.
[7] Disorders and substances that impair circulation contribute, including diabetes, Raynaud's phenomenon, tobacco and alcohol use.
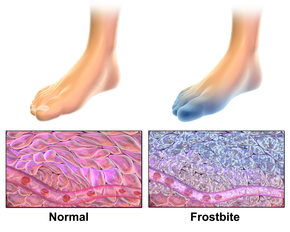
[14] Rewarming causes tissue damage through reperfusion injury, which involves vasodilation, swelling (edema), and poor blood flow (stasis).
This slower temperature decrease allows the body to try to compensate through alternating cycles of closing and opening blood vessels (vasoconstriction and vasodilation).
Small clots (microthrombi) form and can cut off blood to the affected area (known as ischemia) and damage nerve fibers.
Rewarming causes a series of inflammatory chemicals such as prostaglandins to increase localized clotting.
[19] The Wilderness Medical Society recommends covering the skin and scalp, taking in adequate nutrition, avoiding constrictive footwear and clothing, and remaining active without causing exhaustion.
[7] Active rewarming seeks to warm the injured tissue as quickly as possible without burning.
[22] According to Handford and colleagues, "The Wilderness Medical Society and State of Alaska Cold Injury Guidelines recommend a temperature of 37–39 °C, which decreases the pain experienced by the patient whilst only slightly slowing rewarming time."
[24] In addition to vasodilators, sympatholytic drugs can be used to counteract the detrimental peripheral vasoconstriction that occurs during frostbite.
Debridement or amputation of necrotic tissue is usually delayed unless there is gangrene or systemic infection (sepsis).
The classification system of grades, based on the tissue response to initial rewarming and other factors is designed to predict degree of longterm recovery.
These include transient or permanent changes in sensation, paresthesia, increased sweating, cancers, and bone destruction/arthritis in the area affected.
Research suggests that men aged 30–49 are at highest risk, possibly due to occupational or recreational exposures to cold.
[11] Researchers have found evidence of frostbite in humans dating back 5,000 years, in an Andean mummy.
[11] Several notable cases of frostbite include: Evidence is insufficient to determine whether or not hyperbaric oxygen therapy as an adjunctive treatment can assist in tissue salvage.
[28] Studies have suggested that administration of tissue plasminogen activator (tPa) either intravenously or intra-arterially may decrease the likelihood of eventual need for amputation.