Gingival sulcus
A healthy sulcular depth is three millimeters or less, which is readily self-cleansable with a properly used toothbrush or the supplemental use of other oral hygiene aids.
Otherwise, the lone standing tooth will be included with the recordings of the adjacent sextant.Usually, radiographs would be taken to evaluate alveolar bone levels for teeth or sextants where BPE codes 3 or 4 are found assuming no false pockets.
[4][5][6] In clinical gingival health, homeostasis occurs because resident biofilm of plaque bacteria and the host defences (symbiosis) results in a dynamic equilibrium with oral hygiene practices such as brushing and flossing.
Therefore, despite having clinical gingival health, a low level of inflammatory infiltrate, consisting of neutrophils, B Cell Lymphocytes and macrophages, is always present in the connective tissue underlying the junctional epithelium.
The constant low-level inflammatory reaction in the connective tissue underlying the junctional epithelium also results in the formation of the Gingival Crevicular Fluid (GCF).
Dissimilarly to dental caries, many bacteria associated to periodontal disease cannot metabolise carbohydrates for energy (they are asaccharolytic) and are proteolytic too.
The changes in the ecology of the gingival sulcus impacts gene expression and changes the competitiveness of periodontal pathogens like Porphyromonas gingivalis.
Hence, the growth of proteolytic and Gram-Negative Anaerobes (most of the time) will be favoured by fluctuating homeostasis, the natural balance, of the subgingival microflora.
In a perfect scenario, the sample should be taken as close to the expanding front of the lesion as possible to exclude any organisms which are not involved in tissue destruction and to achieve a clear connection between the disease activity and specific bacteria.
If accumulated microbes remain undisturbed in a sulcus for an extended period of time, they will penetrate and ultimately destroy the delicate soft tissue and periodontal attachment fibers.
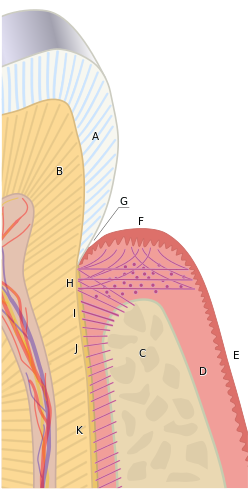
B) Root of the tooth, covered by cementum
C) Alveolar bone
D) Subepithelial connective tissue
E) Oral epithelium
F) Free gingival margin
G) Gingival sulcus
H) Principal gingival fibers
I) Alveolar crest fibers of the periodontal ligament (PDL)
J) Horizontal fibers of the PDL
K) Oblique fibers of the PDL
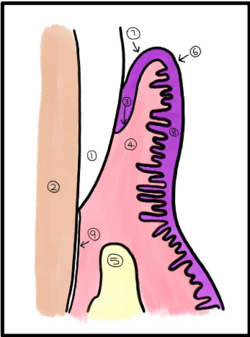
2) Dentin
3) Junctional epithelium
4) Connective tissue
5) Alveolar bone
6) Gingival margin
7) Sulcular epithelium
8) Gingival epithelium
9) Cementum



2) Tooth enamel
3) Infiltrated connective tissue (is this the pink dots – surely they should be under the junctional epithelium rather than at the gingival crest
4) Gingival sulcus
5) Microbial colonization
6) Dental plaque and biofilm
7) Junctional epithelium: base of gingival sulcus