Health equity
[16] Because one's job or career is a primary conduit for both financial and social capital, work is an important, yet underrepresented, factor in health inequities research and prevention efforts.
[19][20][21] In China, for instance, the collapse of the Cooperative Medical System left many of the rural poor uninsured and unable to access the resources necessary to maintain good health.
[25] The segregation of communities on the basis of income occurs in nations worldwide and has a significant impact on quality of health as a result of a decrease in social capital for those trapped in poor neighborhoods.
[37] There is also evidence for a correlation between socioeconomic status and health literacy; one study showed that wealthier Tanzanian families were more likely to recognize disease in their children than those that were coming from lower income backgrounds.
In 2019, the federal government identified nearly 80 percent of rural America as "medically underserved," lacking in skilled nursing facilities, as well as rehabilitation, psychiatric and intensive care units.
[53][54] A 2023 scoping review of the literature found that in studies involving multiracial or multiethnic populations, the incorporation of race or ethnicity variables lacked thoughtful conceptualization and informative analysis concerning their role as indicators of exposure to racialized social disadvantage.
[66][67] In South America, indigenous populations faced similarly poor health outcomes with maternal and infant mortality rates that were significantly higher (up to 3 to 4 times greater) than the national average.
[70] On February 5, 2021, the head of the World Health Organization (WHO), Tedros Adhanom Ghebreyesus, noted regarding the global inequity in the access to COVID-19 vaccines, that almost 130 countries had not yet given a single dose.
[79] In developing countries, males tend to have a health advantage over women due to gender discrimination, evidenced by infanticide, early marriage, and domestic abuse for females.
[81] Women are generally are of lower socioeconomic status (SES) in USA and have more barriers to accessing healthcare, and higher rates of depression and chronic stress and negative impact health.
[87] Millions of individuals living in rural areas in the United States are more at risk of having decreased access to maternal health care facilities if the community is low-income.
Homosexual, bisexual, transgender, and gender-variant populations around the world experience a range of health problems related to their sexuality and gender identity,[104][105][106][107] some of which are complicated further by limited research.
[114] This discrimination can take the form of verbal abuse, disrespectful conduct, refusal of care, the withholding of health information, inadequate treatment, and outright violence.
[114][115] Additionally, members of the LGBT community contend with health care disparities due, in part, to lack of provider training and awareness of the population's healthcare needs.
[115] As a component of this fact, medical schools do not focus much attention on LGBT health issues in their curriculum; the LGBT-related topics that are discussed tend to be limited to HIV/AIDS, sexual orientation, and gender identity.
The causes of these health inequities are "i) cultural and social norms that preference and prioritise heterosexuality; ii) minority stress associated with sexual orientation, gender identity and sex characteristics; iii) victimisation; iv) discrimination (individual and institutional), and; v) stigma.
"[128] Minority populations have increased exposure to environmental hazards that include lack of neighborhood resources, structural and community factors as well as residential segregation that result in a cycle of disease and stress.
[130] In addition, minority neighborhoods have various health hazards that result from living close to highways and toxic waste factories or general dilapidated structures and streets.
[130] These environmental conditions create varying degrees of health risk from noise pollution, to carcinogenic toxic exposures from asbestos and radon that result in increase chronic disease, morbidity, and mortality.
This group is exposed to high levels of particulate matter and pesticides on the job, which have contributed to increased cancer rates, lung conditions, and birth defects in their communities.
[135] Racial segregation is another environmental factor that occurs through the discriminatory action of those organizations and working individuals within the real estate industry, whether in the housing markets or rentals.
[136] Thus, segregation results in minorities clustering in poor neighborhoods that have limited employment, medical care, and educational resources, which is associated with high rates of criminal behavior.
[137][138] In addition, segregation affects the health of individual residents because the environment is not conducive to physical exercise due to unsafe neighborhoods that lack recreational facilities and have nonexistent park space.
[175] Patient health decisions can be influenced by religious beliefs, mistrust of Western medicine, and familial and hierarchical roles, all of which a white provider may not be familiar with.
[185] In the UK, Public Health England, a universal service free at the point of use, which forms part of the NHS, offers regular screening to any member of the population considered to be in an at-risk group (such as individuals over 45) for major disease (such as colon cancer, or diabetic-retinopathy).
[186][187] There are a multitude of strategies for achieving health equity and reducing disparities outlined in scholarly texts, some examples include: In 2023, the G20 under its Affordable Healthcare Model Hospital initiative, with the Government of Andhra Pradesh, India, opened a 100-bed facility in Srikakulam, drawing support from the Aarogyasri scheme.
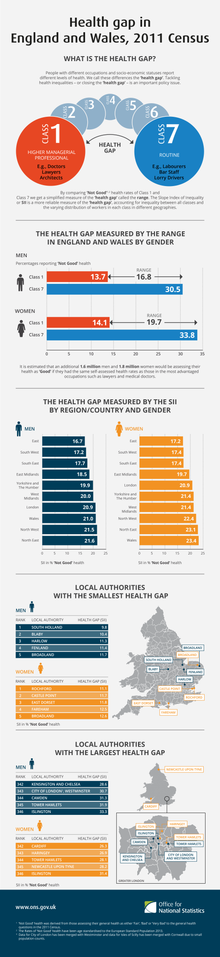
On 11 February 2010, Sir Michael Marmot, an epidemiologist at University College London, published the Fair Society, Healthy Lives report on the relationship between health and poverty.
In its report on this study, The Economist argued that the material causes of this contextual health inequality include unhealthful lifestyles – smoking remains more common, and obesity is increasing fastest, amongst the poor in Britain.
For example, limitations in public health surveys in the United States to collect data on race, ethnicity, and nativity; (2) Institutionalized exclusion – codification of exclusionary social structures in research practices, instruments, and scientific models resulting in an inherent bias in favor of the normative group.
For example, the definition of a human as an 80 kg man in toxicology; (3) Unexamined assumptions – cultural norms and unconscious bias that can impact all aspects of research.