Healthcare in Pakistan
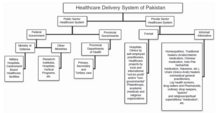
Health care delivery has traditionally been jointly administered by the federal and provincial governments with districts mainly responsible for implementation.
The private health sector constitutes a diverse group of doctors, nurses, pharmacists, traditional healers, drug vendors, as well as laboratory technicians, shopkeepers and unqualified practitioners.
Due to the absence of these institutions and the cost associated with transportation, impoverished people living in rural and remote areas tend to consult private doctors.
[4][10] The private health sector operates through a fee-for-service system of unregulated hospitals, medical practitioners, homeopathic doctors, hakeems, and other spiritual healers.
Urbanisation and an unhealthy, energy-dense diet (the high presence of oil and fats in Pakistani cooking), as well as changing lifestyles, are among the root causes contributing to obesity in the country.
[22] Additionally, at the “national level almost 40% of these children are underweight...and about 9% [are affected] by wasting”, diseases where muscle and fat tissues degenerate as a result of malnutrition.
[23] Similarly, approximately 42 % of women in Pakistan in reproductive age are anemia as per National Nutritional Survey-2018,[24] with a slightly higher percentage in villages than in urban areas.
[26] This in turn can be attributed in part to the rapid urbanisation and mass migrations caused by the Great Partition of India and Pakistan, and the resulting issues with infrastructure and government, as well as other factors.
According to the United Nations Population Fund unmet access to sexual and reproductive health deprive women of the right to make crucial choices about their bodies and future and affect the family welfare.
Poor reproductive health of adolescents leads to early childbearing and parenthood, pregnancy complications, maternal deaths and disability.
Adolescents and youth face barriers in accessing sexual and reproductive health services such as needing an elder family member to accompany them.
Further country's socio-cultural background discourages the discussion about reproductive health, making it difficult to provide sex education and awareness about sexually transmitted diseases.
According to latest Pakistan Demographic and Health Survey 2017–18 the proportions of young married men and women who have heard about HIV/AIDS or have comprehensive knowledge about it are quite low.
Even when patients recognize their symptoms, overcome the stigma, gain the support of their families and start looking for medical help, there are insufficient mental healthcare facilities.
[40][55] It is concluded that the health care system's response in Pakistan is not adequate to meet the current challenges and that changes in policy are needed.
[49] Political commitment, adequate human and financial resources, and advocacy are needed for the integration of mental health into PHC in Pakistan.
These programmes have been found effective in reducing stigma and increase awareness of mental illness amongst the adults and children living in rural areas.
It will call for improving political commitments and help develop policies, and legislative infrastructure, to provide integrated health care.
[54] The British BasicNeeds program, mental health focused international NGO with a global reach spanning 14 countries, began forming partnerships with Pakistani nonprofits in 2013, has already served 12,000 people in need of psychiatric attention.
In addition to setting up camps where patients can see doctors, receive prescriptions for medicines and engage in therapy, the program trains citizens to recognise symptoms and side effects of mental illnesses.
[55][58] According Dr Nasir Javed Malik, there are 274,135 doctors (2022 Statistics from Pakistan Medical Commission) and 14,568 health care facilities in 2021–22 to cater for over 229 million people.
The four-year training culminates in achieving a Bachelor of Dental Surgery (BDS) degree, which requires a further one year compulsory internship to be a registered dentist in Pakistan.
Currently Pakistan has more than 800 large volume pharmaceutical formulation units, including those operated by 25 multinationals present in the country.
Specialized finished dosage forms such as soft gelatin capsules, parenteral fat emulsions and Metered-dose inhalers continue to be imported.
Currently the industry has the capacity to manufacture a variety of traditional products ranging from simple pills to capsules, ointments and syrups.
Medical tourism in Pakistan is viewed as an untapped market that could be turned into a huge opportunity if the government "focuses on key issues".
A number of modern hospital facilities exist in major cities such as Islamabad, Karachi and Lahore that are fully equipped and facilitated with the latest medical technologies.
The main goal of the program is to provide primary health care to underserved populations, particularly women and children, through family planning services.
[63] The main responsibilities of lady health workers are to conduct screenings of pregnant women and refer them to clinical services if needed, distribute condoms and contraceptive pills, provide interventions for malnutrition such as nutritional counseling, and treat common diseases with special drug kits.
Other possible improvements include skill and career development opportunities for lady health workers and a stronger patient referral system within the program.