Healthcare in Europe
Healthcare in Europe is provided through a wide range of different systems run at individual national levels.
Most European countries have a system of tightly regulated, competing private health insurance companies, with government subsidies available for citizens who cannot afford coverage.
[5] According to the European Health Interview Survey (EHIS) conducted between 2013 and 2015, substantial inequalities existed in terms of sex, age and education level concerning the proportion of adults who were daily smokers of cigarettes.
The European Commission's Directorate-General for Health and Consumers however seeks to align national laws on the safety of food and other products, on consumers' rights, and on the protection of people's health, to formulate new EU wide laws and thus strengthen its internal markets.
In responding to the COVID-19 pandemic, public health infrastructures and resources, governmental, and cultural values all play a key role in stopping the threat.
Finding an approach that balances effectiveness, efficiency, and successful response to the pandemic is the key to ending the crisis.
The governmental response including the banning of all international non-essential travel and COVID-19 lockdowns helped to keep the death toll to a minimum.
The Public Health Agency of Sweden proposed a ban on gatherings over 500 people, including social distancing.
[13] Triaging issues that determined medical priority to increase survival rates from COVID-19 contrasted between Sweden and Greece.
This caused a fundamental collapse of the healthcare system, needless deaths, and a misinformed and distrusting public that demanded more accountability from the European Union members, the government, and health professionals.
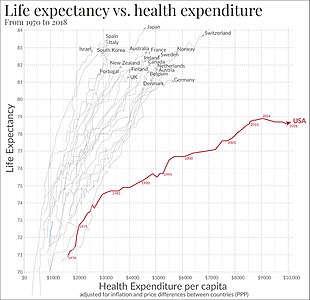
For example, Eastern Europe is a low-income region, with a lower life expectancy due to biological factors including genetics, nutrition, and even hormonal issues.
Another non-biological factor that cooperates with the decrease in life expectancy in Eastern Europe would be unhealthy stress that affects cardiovascular health.
According to a new study published by the Smithsonian Magazine by the author Ridhi Kashyap, an associate professor of social demography at the University of Oxford.
[17] Due to the high demand on hospitals, the vaccines served as a mechanism to decrease the load on doctors and medics.