Hemolysis
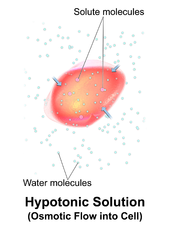
Hemolysis inside the body can be caused by a large number of medical conditions, including some parasites (e.g., Plasmodium), some autoimmune disorders (e.g., autoimmune haemolytic anaemia, drug-induced hemolytic anemia, atypical hemolytic uremic syndrome (aHUS)[4]),[5] some genetic disorders (e.g., Sickle-cell disease or G6PD deficiency), or blood with too low a solute concentration (hypotonic to cells).
[8] Because in vivo hemolysis destroys red blood cells, in uncontrolled, chronic or severe cases it can lead to hemolytic anemia.
[16] As a result, the contents of the red blood cell are released into the general circulation, leading to hemoglobinemia[17] and increasing the risk of ensuing hyperbilirubinemia.
[18] Intravascular hemolysis may occur when red blood cells are targeted by autoantibodies, leading to complement fixation, or by damage by parasites such as Babesia.
[24] If extravascular hemolysis is extensive, hemosiderin can be deposited in the spleen, bone marrow, kidney, liver, and other organs, resulting in hemosiderosis.
[27] Excessive suction can cause the red blood cells to be smashed on their way through the hypodermic needle owing to turbulence and physical forces.
Such hemolysis is more likely to occur when a patient's veins are difficult to find or when they collapse when blood is removed by a syringe or a modern vacuum tube.
In vitro hemolysis during specimen collection can cause inaccurate laboratory test results by contaminating the surrounding plasma with the contents of hemolyzed red blood cells.
Modeling of fluid flows to predict the likelihood of red cell membrane rupture in response to stress is an active area of research.
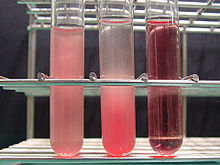
[28] Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various Gram-positive bacteria infections (e.g., Streptococcus).
[32] This can lead to esophageal spasm and dysphagia, abdominal pain, erectile dysfunction, systemic hypertension, decreased organ perfusion, promotion of inflammation and coagulation, and thrombosis.