Hypoalbuminemia
Alternatively, it can present with death in utero prior to birth or as a disease of adults characterized by edema, fatigue, and hyperlipidemia.
[7] Often, the cause is multifactorial as in liver cirrhosis, where reduced hepatic synthesis and increased capillary leakage combine to further decrease albumin levels.
This is in contrast to acute phase reactants like C-reactive protein (CRP), whose levels increase with inflammatory processes.
With respect to mechanism, inflammation leads to decreased production of albumin as a result of increased levels of cytokines, specifically IL-1, IL-6, and TNF-α.
[8] Hypoalbuminemia can also present as part of the nephrotic syndrome, in which significant quantities of protein are lost in the urine due to kidney damage.
[3] In children, nephrotic syndrome is commonly a primary disease process that is largely idiopathic, although more genetic causes are being identified with the cost and accessibility of whole exome sequencing.
After renal biopsy, these syndromes are commonly diagnosed as minimal change disease, membranoproliferative glomerulonephritis, or focal segmental glomerulosclerosis.
[9] In adults, on the other hand, nephrotic syndrome is commonly a secondary disease process due to a variety of inciting factors.
[3] Albuminuria and resultant hypoalbuminemia can also occur in chronic kidney disease without protein loss levels as high as seen in nephrotic syndrome.
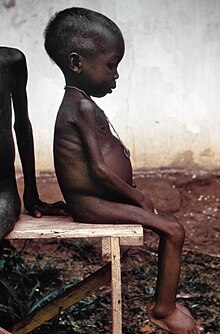
[5] Kwashiorkor is a disease of malnutrition characterized by decreased protein intake and amino acid deficiency resulting in hypoalbuminemia and a characteristic physical presentation.
These functions include regulation of colloid osmotic pressure or protein concentration within the blood plasma, transport of free fatty acids and other molecules to the liver (unconjugated bilirubin, metals, ions) for storage or utilization, binding of drugs and alteration of pharmacokinetics (half-life, biological activity levels, metabolism), buffering plasma pH, scavenging reactive oxygen species to avoid inflammation and associated damage, functioning as a reservoir of nitric oxide for the regulation of blood pressure, and prevention of coagulation and platelet aggregation in an action similar to the commonly used anticoagulant heparin.
In kidney disease, a CMP may be ordered as a follow-up test when proteinuria is detected by urine dipstick analysis, which may lead to a diagnosis of hypoalbuminemia.
[7] Albumin infusions can and are commonly performed although they are expensive and have not been shown to be more effective than colloid solutions in a number of conditions and situations.
Examples of indications for albumin infusion include hypoalbuminemia in the context of major surgery such as hepatic resection >40%, nephrotic syndrome in conjunction with diuretics and corticosteroids, spontaneous bacterial peritonitis in combination with antibiotics, and rapidly progressing hepatorenal syndrome (type 1) in combination with terlipressin.
[7] These indications have shown positive outcomes respective to their diseases, while conditions like malnourishment, burns (during the first 24 hours), and shock with traumatic brain injury either show no benefit or harm in randomized controlled trials.
[8] In disease states specifically, hypoalbuminemia has been used a predictive factor for poor outcomes in a number of conditions,[3] including periprosthetic joint infection treatment failure,[13] and cirrhosis.
[14] In chronic kidney disease, hypoalbuminemia is an indicator of frailty, which is itself associated with complications, mental distress, quality of life impairment, resource utilization, and mortality.