Lacunar stroke
He observed "lacunae" (empty spaces) in the deep brain structures after occlusion of 200–800 μm penetrating arteries and connected them with five classic syndromes.
These syndromes are still noted today, though lacunar infarcts are diagnosed based on clinical judgment and radiologic imaging.
This type of stroke often causes lesions in the surrounding brain tissue that are visibly detected via neuroimaging techniques such as MRI and computed axial tomography (CT scan).
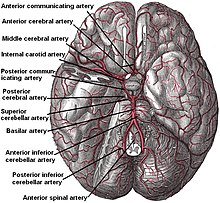
Other lesions that are associated with lacunes appear in the "deep nuclei of the brain (37% putamen, 14% thalamus, and 10% caudate) as well as the pons (16%) or the posterior limb of the internal capsule (10%)".
These lesions are less common within other brain regions such as the cerebellum, cerebral white matter and anterior limb of the internal capsule.
The most current theory indicates endothelial dysfunction and increased permeability of the blood-brain barrier first allow leakage of blood contents, promoting gliosis and white matter hyper-intensities on magnetic resonance imaging.
Moreover, focal narrowing of brain vessels and impairment of their ability to dilate in response to various stimuli may lead to a decreased cerebral blood flow and ultimately lacunar stroke.
Typically, tissue plasminogen activator may be administered within 3 to 4.5 hours of stroke onset if the patient is without contraindications (i.e. a bleeding diathesis such as recent major surgery or cancer with brain metastases).
For long term prevention of recurrence, medical regimens are typically aimed towards correcting the underlying risk factors for lacunar infarcts such as hypertension, diabetes mellitus and cigarette smoking.