Maternal mortality in India
India is a signatory to the Millennium Declaration adopted at the United Nations General Assembly in September 2000, and consistently reaffirmed its commitment towards the eight development goals.
[14] The first report on maternal mortality in India (1997-2003), describing trends, causes and risk factors, was released in October 2006.
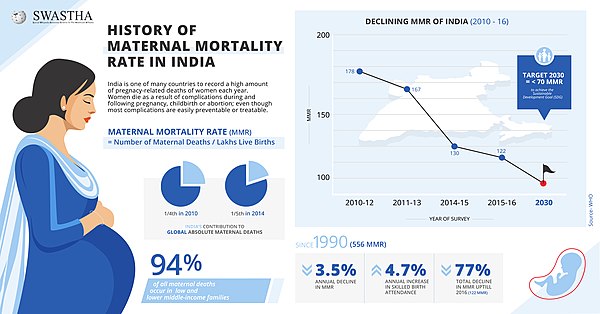
Statistics showed that up until 2010, more than half a million women—most of them living in developing countries—dies from pregnancy- or childbirth-related complications every year, and about a quarter of these “maternal” deaths occurred in India.
[17] As per Sample Registration System (SRS), 2011-13 reports published by Registrar General of India, Maternal Mortality Ratio (MMR) was 167 per 1,00,000 live births in the country.
[22] Approximately two-thirds of all maternal deaths are primarily caused by major complications, including severe bleeding (typically occurring after childbirth), infections (commonly arising after childbirth), high blood pressure during pregnancy (pre-eclampsia and eclampsia), delivery-related complications, and unsafe abortions.
[23] Between 50% and 98% of maternal deaths result from direct obstetric causes such as hemorrhage, infection, hypertensive disorders, ruptured uterus, hepatitis, and anemia.
According to the National Health Policy (NHP) 2017, India set a goal to reduce its Maternal Mortality Rate (MMR) to below 100 per lakh live births by the year 2020.
Kerala, Maharashtra and Tamil Nadu have already met the sustainable development goals target of 70 per 100,000 MMR, while Andhra Pradesh and Telangana are within range.
[34] In the recently released report on maternal mortality ratio (MMR) prepared by the union government, Uttarakhand has fared significantly well recording 89 deaths per lakh deliveries between 2015 and 2017 as against the national average of 122.
Pregnant women are provided special, free ante-natal checks in their second or third trimester at government health care facilities, including ultrasounds, blood and urine tests.
[37] Full ANC refers to at least four antenatal visits, one tetanus toxoid (TT) injection and iron folic acid tablets or syrup taken for 100 or more days.
[40] A regional program in Andhra Pradesh seeks to ask doctors and nurses about the causes of maternal mortality in local communities.
[46] Various civil organizations have suggested effective strategies for reducing MMR in India: In 2018 the World Health Organization noted four recent changes in India which had lowered maternal mortality:[47] Before 2017 the government focus on maternal mortality was learning about the causes of death to develop a plan for prevention.
[49] Contrary to expectation, the study instead found that after a maternal death, women instead avoid hospitals and instead seek support from a traditional birth attendant.
[citation needed] The same health monitoring systems which track maternal mortality could also ask women to report other problems, such as lack of good treatment from hospital staff.
[citation needed] The Government of India has started various public health initiatives to provide a safe and secure environment.
[60] For the earlier 2013 versions of these two studies, researchers noted that they used different data and analysis to come to different conclusions about changes over time of maternal mortality in India.
[61] In 2017 a report found no significant impact following a large study of 160,000 pregnant women who participated in a one-week educational program to improve maternal health and childbirth outcomes.