Maternal mortality in the United States
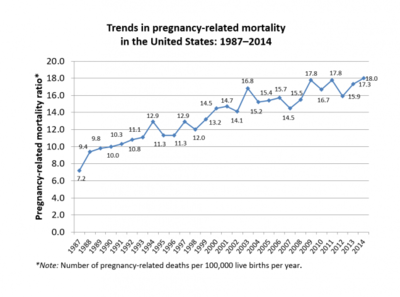
[8] In 1986, the Centers for Disease Control and Prevention (CDC) and the American College of Obstetricians and Gynecologists (ACOG) created the Pregnancy-Related Mortality Surveillance System to monitor maternal deaths during pregnancy and up to one year after giving birth.
[11] After decades of inaction on the part of the U.S. Congress towards reducing the maternal mortality ratio, the United States Senate Committee on Appropriations voted on June 28, 2018, to request $50 million to prevent the pregnancy-related deaths of American women.
In 2019, Black maternal health advocate and Parents writer Christine Michel Carter interviewed Vice President Kamala Harris.
Harris stated:"We need to speak the uncomfortable truth that women—and especially Black women—are too often not listened to or taken seriously by the health care system, and therefore they are denied the dignity that they deserve.
And we need to speak this truth because today, the United States is 1 of only 13 countries in the world where the rate of maternal mortality is worse than it was 25 years ago.
It also meant that for many years, the United States could not report a national maternal mortality rate to the OECD or other repositories that collect data internationally.
[6][15]: 427 In response to the MacDorman study, revealing the "inability, or unwillingness, of states and the federal government to track maternal deaths",[16] ProPublica and NPR found that in 2016 alone, between 700 and 900 women died from pregnancy- and childbirth-related causes.
[17] According to a 2009 article in Anthropology News, studies conducted by but not limited to Amnesty International, the United Nations, and federal programs such as the CDC, maternal mortality has not decreased since 1999 and may have been rising.
New York's panel, the Maternal Mortality and Morbidity Review Committee (M3RC), included doctors, nurses, "doulas, midwives and social workers".
[19] In July 2018, New York City's de Blasio's administration announced that it would be allocating $12.8 million for the first three years of its five-year plan to "reduce maternal deaths and life-threatening complications of childbirth among women of color".
[21] The World Health Organization and the CDC's National Vital Statistics System (NVSS) define maternal death as that which occurs within the first 42 days after birth.
Since 1986, the Center for Disease Control conducts a Pregnancy Mortality Surveillance Service (PMSS) to study the medical causes of maternal death.
According to a 2020 study conducted by Erica L. Eliason, cutting Medicaid funding limits access to prenatal healthcare, which has been shown to increase maternal mortality rates.
[27] A 2012 national survey by Childbirth Connection found that women using Medicaid to pay for birth expenses were twice as likely as those using private insurance to have never heard of a doula (36% vs.
[35] This high risk can be accounted for by various causes such as the likelihood of adolescents giving birth for the first time compared to women in older age groups.
[40] Maternal adverse outcomes include delayed or insufficient prenatal case, poor weight gain, and an increase in nicotine, alcohol and substance abuse.
The same survey revealed that Black and Hispanic mothers were nearly three times more likely to experience discrimination in the healthcare system due to their race, language or culture.
The VBAC calculator also has two race based correction factors, for African American and Hispanic patients, that “subtract” from the likelihood of successful vaginal birth.
The VBAC calculator was endorsed by the National Institute of Child Health and Human Development, and was created in attempts to assist providers in their risk assessment for a patient's vaginal birth plan.
This calculator accounts for various risk factors, including age, BMI, and previous health complications, which could have impacts on a woman's birth outcomes.
[52] Subjecting people of color as ineligible to receiving the safer pregnancy outcome can be highly detrimental to the safety of some pregnant patients.
In fact, the calculator includes a new, more objective clinical variable: whether or not a patient has been treated for chronic hypertension, which can impact the amount of blood flow to the placenta.
Some other risk factors include obesity, chronic high blood pressure, increased age, diabetes, cesarean delivery, and smoking.
[32] Researchers have found that another factor contributing to the elevated maternal mortality rates in the United States is the lack of attention given to black women during childbirth and the failure to recognize preexisting health conditions like diabetes and hypertension, which can cause preeclampsia and eclampsia.
[65] Living in poverty does increase the chances of maternal mortality because women and children do not have the finances to travel to areas in Georgia that have healthcare access.
They reported that the "rate of life-threatening complications for new mothers in the U.S. has more than doubled in two decades due to pre-existing conditions, medical errors and unequal access to care.
"[82] According to the Centers for Disease Control and Prevention, c. 4 million women who give birth in the US annually, over 50,000 a year, experience "dangerous and even life-threatening complications.
"[82] According to a report by the United States Centers for Disease Control and Prevention, in 1993 the rate of Severe Maternal Morbidity, rose from 49.5 to 144 "per 10,000 delivery hospitalizations" in 2014, an increase of almost 200 percent.
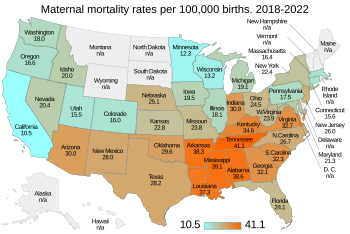
[4] Deaths per 100,000 live births There are many possible reasons why the United States has a much larger MMR than other developed countries: many hospitals are unprepared for maternal emergencies, 44% of maternal-fetal grants do not go towards the health of the mother, and pregnancy complication rates are continually increasing.
A recent report from the US Centers for Disease Control and Prevention (CDC) showed that maternal mortality – deaths that occur during pregnancy or within 42 days after delivery – increased by 40% in 2021.