Medial knee injuries
[1][3] A thorough understanding of the anatomy and function of the medial knee structures, along with a detailed history and physical exam, are imperative to diagnosing and treating these injuries.
[7] As with all surgeries, there is a risk of bleeding, wound problems, deep vein thrombosis, and infection that can complicate the outcome and rehabilitation process.
The long term complication of arthrofibrosis and heterotopic ossification (Pellegrini-Stieda syndrome) are problems that are best addressed with early range of motion and following defined rehabilitation protocols.
[4][5][6][8] Failure of graft due to intrinsic mechanical forces should be prevented with preoperative alignment assessment (osteotomy treatment) and proper rehabilitation.
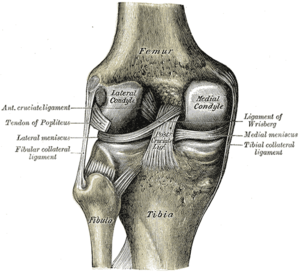
[2][9] The dMCL connects directly to the medial meniscus and therefore can be divided into meniscofemoral and meniscotibial ligament components.
The POL (called by older texts: oblique portion of the sMCL) is a fascial expansion with three main components: superficial, central (tibial), and capsular.
[2][10] It arises from the semimembranosus tendon and connects anterior and distal to the gastrocnemius tubercle via the posterior joint capsule.
[3][4][11] The MPFL arises from the fibers of the vastus medialis obliquus muscle and attaches distally to the superior medial aspect of the patella.
[2] It has a fascial expansion on the distal-medial aspect that attaches to the medial gastrocnemius tendon, capsular arm of the POL, and posteromedial joint capsule.
The vastus medialis obliquus muscle courses over the anteromedial thigh, attaching along the adductor magnus anterior border and to the quadratus femoris tendon.
The practitioner should also evaluate the contralateral (non-injured) knee to note any differences in gross appearance and landmarks.
Grade II injuries have broad tenderness over the medial knee and have some gapping with a firm end-point during valgus testing; this represents a partial tear of the ligaments.
[15] LaPrade et al. reported, however, that a simulated grade III sMCL injury showed only 3.2 mm of increased medial compartment gapping compared to the intact state.
Bilateral valgus stress AP images can show a difference in medial joint space gapping.
This finding is due to calcification of the sMCL (heterotopic ossification) caused by the chronic tear of the ligament.
[5][16] Magnetic resonance imaging (MRI) can be helpful in assessing for a ligamentous injury to the medial side of the knee.
[6][21] The consensus of many studies is that isolated grade I, II, and III injuries are usually well suited to non-operative treatment protocols.
[22] Protection can be performed using a hinged brace that stabilizes against varus and valgus stress but allows full flexion and extension.
The brace should be worn for the first four to six weeks of rehabilitation, especially during physical exercise to prevent trauma to the healing ligament.
The typical return-to-play time frame for most athletes with a grade III medial knee injury undergoing a rehabilitation program is 5 to 7 weeks.
[4][23][5][14] It has been reported that severe acute and chronic grade III medial knee injuries often involve the sMCL in combination with the POL.
[10][24] Direct surgical repair or reconstruction, therefore, should be performed for both of these ligaments because they both play an important role in static medial knee stability.
[26][27] Surgery involving direct repair (with or without augmentation from a hamstring autograft), among other previously used techniques, have not been biomechanically tested.
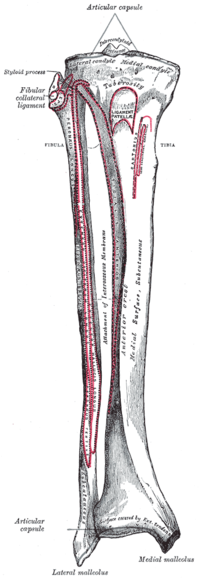
[27] Within the distal borders of the incision, the semitendinosus and gracilis tendons are found beneath the sartorius muscle fascia.
This attachment is exposed by making a small incision parallel to the fibers along the posterior edge of the anterior arm of the semimembranosus tendon.
The sMCL and POL grafts are pulled into their respective femoral tunnels and each secured with a cannulated bioabsorbable screw.
Making sure the tibia remains in neutral rotation, a varus force is used to ensure there is no medial compartment gapping of the knee.
[27] Future research with regard to medial knee injuries should evaluate clinical outcomes between different reconstruction techniques.