Meningitis
[2][8] A lumbar puncture, in which a needle is inserted into the spinal canal to collect a sample of cerebrospinal fluid (CSF), can diagnose or exclude meningitis.
[16] The classic triad of diagnostic signs consists of neck stiffness, sudden high fever, and altered mental status; however, all three features are present in only 44–46% of bacterial meningitis cases.
Other features that distinguish meningitis from less severe illnesses in young children are leg pain, cold extremities, and an abnormal skin color.
[18] The rash consists of numerous small, irregular purple or red spots ("petechiae") on the trunk, lower extremities, mucous membranes, conjunctiva, and (occasionally) the palms of the hands or soles of the feet.
The infection may trigger sepsis, a systemic inflammatory response syndrome of falling blood pressure, fast heart rate, high or abnormally low temperature, and rapid breathing.
Endocarditis (an infection of the heart valves which spreads small clusters of bacteria through the bloodstream) may cause aseptic meningitis.
[2] An infection in the head and neck area, such as otitis media or mastoiditis, can lead to meningitis in a small proportion of people.
[31] Recurrent bacterial meningitis may be caused by persisting anatomical defects, either congenital or acquired, or by disorders of the immune system.
[34] There are a number of risk factors for fungal meningitis, including the use of immunosuppressants (such as after organ transplantation), HIV/AIDS,[35] and the loss of immunity associated with aging.
[42] Other less common pathogenic fungi which can cause meningitis include: Coccidioides immitis, Histoplasma capsulatum, Blastomyces dermatitidis, and Candida species.
[4] The meninges comprise three membranes that, together with the cerebrospinal fluid, enclose and protect the brain and spinal cord (the central nervous system).
[2] Direct contamination of the cerebrospinal fluid may arise from indwelling devices, skull fractures, or infections of the nasopharynx or the nasal sinuses that have formed a tract with the subarachnoid space (see above); occasionally, congenital defects of the dura mater can be identified.
The blood–brain barrier becomes more permeable, leading to "vasogenic" cerebral edema (swelling of the brain due to fluid leakage from blood vessels).
[2] Administration of antibiotics may initially worsen the process outlined above, by increasing the amount of bacterial cell membrane products released through the destruction of bacteria.
[47] There are no specific signs or symptoms that can indicate meningitis, and a lumbar puncture (spinal tap) to examine the cerebrospinal fluid is recommended for diagnosis.
[51] The cause of hyponatremia, however, is controversial and may include dehydration, the inappropriate secretion of the antidiuretic hormone (SIADH), or overly aggressive intravenous fluid administration.
Neutrophil granulocytes tend to have migrated to the cerebrospinal fluid and the base of the brain, along with cranial nerves and the spinal cord, may be surrounded with pus – as may the meningeal vessels.
[59][68] The pneumococcal polysaccharide vaccine, which covers 23 strains, is only administered to certain groups (e.g. those who have had a splenectomy, the surgical removal of the spleen); it does not elicit a significant immune response in all recipients, e.g. small children.
In cases of meningococcal meningitis, preventative treatment in close contacts with antibiotics (e.g. rifampicin, ciprofloxacin or ceftriaxone) can reduce their risk of contracting the condition, but does not protect against future infections.
[69] While antibiotics are frequently used in an attempt to prevent meningitis in those with a basilar skull fracture there is not enough evidence to determine whether this is beneficial or harmful.
[3] Hydrocephalus (obstructed flow of CSF) may require insertion of a temporary or long-term drainage device, such as a cerebral shunt.
[72] Empiric antibiotics (treatment without exact diagnosis) should be started immediately, even before the results of the lumbar puncture and CSF analysis are known.
[8] In young children and those over 50 years of age, as well as those who are immunocompromised, the addition of ampicillin is recommended to cover Listeria monocytogenes.
[8][48] Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens.
[74] Additional treatment with corticosteroids (usually dexamethasone) has shown some benefits, such as a reduction of hearing loss, and better short term neurological outcomes[75] in adolescents and adults from high-income countries with low rates of HIV.
[75] Even in high-income countries, the benefit of corticosteroids is only seen when they are given prior to the first dose of antibiotics, and is greatest in cases of H. influenzae meningitis,[8][79] the incidence of which has decreased dramatically since the introduction of the Hib vaccine.
[3] In children there are several potential disabilities which may result from damage to the nervous system, including sensorineural hearing loss, epilepsy, learning and behavioral difficulties, as well as decreased intelligence.
[91] Meningococcal disease occurs in epidemics in areas where many people live together for the first time, such as army barracks during mobilization, university and college campuses[2] and the annual Hajj pilgrimage.
[92] The description of tuberculous meningitis, then called "dropsy in the brain", is often attributed to Edinburgh physician Sir Robert Whytt in a posthumous report that appeared in 1768, although the link with tuberculosis and its pathogen was not made until the next century.
In 1906, antiserum was produced in horses; this was developed further by the American scientist Simon Flexner and markedly decreased mortality from meningococcal disease.







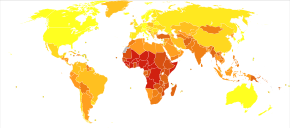
-
no data
-
<10
-
10–25
-
25–50
-
50–75
-
75–100
-
100–200
-
200–300
-
300–400
-
400–500
-
500–750
-
750–1000
-
>1000

-
0–2
-
3-3
-
4–6
-
7–9
-
10–20
-
21–31
-
32–61
-
62–153
-
154–308
-
309–734