Monkeypox virus
[4] Symptoms of mpox in humans include a rash that forms blisters and then crusts over, fever, and swollen lymph nodes.
[10] Members of the poxvirus family, include the monkeypox virus itself have been listed by the WHO as diseases with epidemic or pandemic potential.
[11] The monkeypox virus is listed as being a potentially high or severe threat pathogen in both the European Union (EU) and the United States of America.
[5] MPV is 96.3% identical to the variola virus in regards to its coding region, but it does differ in parts of the genome which encode for virulence and host range.
[20] As an Orthopoxvirus, MPV replication occurs entirely in the cell cytoplasm within 'factories' – created from the host rough endoplasmic reticulum (ER) – where viral mRNA transcription and translation also take place.
[24] The MV of the monkeypox virus has an Entry Fusion Complex (EFC), allowing it to enter the host cell after attachment.
[23] DNA concatemers process the genomes, which appear in new virions, along with other enzymes, and genetic information needed for the replication cycle to occur.
[23] Zoonotic transmission can occur from direct contact with the blood, bodily fluids, wounds, or mucosal lesions of infected animals whether they are dead or alive.
[39] The MVA-BN vaccine, originally developed for smallpox, has been approved in the United States for use by persons who are either considered at high risk of exposure to mpox, or who may have recently been exposed to it.
These include that healthcare providers don a gown, mask, goggles, and a disposable filtering respirator (such as an N95), and that an infected person should be isolated a private room to keep others from possible contact.
[50] Those living in countries where mpox is endemic should avoid contact with sick mammals such as rodents, marsupials, non-human primates (dead or alive) that could harbour Orthopoxvirus monkeypox and should refrain from eating or handling wild game (bush meat).
Viral proteins, expressed by infected cells, employ multiple approaches to limit immune system activity, including binding to, and preventing activation of proteins within the host's immune system, and preventing infected cells from dying to enable them to continue replicating the monkey pox virus.
[63] The CFR of the 2022-2023 global outbreak (caused by clade IIb) has been very low - estimated at 0.16%, with the majority of deaths in individuals who were already immunocompromised.
[64] Central African Monkeypox virus was first identified by Preben von Magnus in Copenhagen, Denmark, in 1958 in crab-eating macaque monkeys (Macaca fascicularis) being used as laboratory animals.
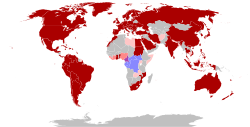
[70] The first reported outbreak in humans outside of Africa occurred in 2003 in the United States; it was traced to Gambian pouched rats which had been imported as exotic pets.
In August 2024 it was reported that the UAE will donate Monkeypox vaccines to the Democratic Republic of Congo, Nigeria, South Africa, Ivory Coast, and Cameroon.