Management of acute coronary syndrome
[2] Acute coronary syndromes are classified to two major categories, according to the patient's electrocardiogram, and specifically the presence or absence of persistent (>20 min) ST segment elevation (or left bundle branch block).
[3] Damage is reversible for approximately 20[4]-30[5] minutes after complete obstruction of blood flow; thereafter myocardial cell death ensues and progresses as time passes.
Therefore, complete and sustained restoration of blood flow must be as prompt as possible to ensure maximum salvage of functional myocardium, a principle expressed in the maxim "time is muscle".
[11][12][13] Patients with known coronary artery disease who have been prescribed nitroglycerin should promptly take one dose, and call emergency medical services if their symptoms do not improve within 2–5 minutes.
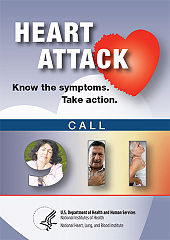
[15] Health care professionals are responsible for teaching their patients at risk of acute coronary syndrome what the symptoms of this condition are, and that it is imperative to seek urgent medical attention in case they present.
[16] Emergency Medical Services (EMS) Systems vary considerably in their ability to evaluate and treat patients with suspected acute myocardial infarction.
[18] If a STEMI is recognized the paramedic may be able to contact the local PCI hospital and alert the emergency room physician, and staff of the suspected AMI.
[25] Even in the absence of a formal alerting program, prehospital 12-lead ECGs are independently associated with reduced door to treatment intervals in the emergency department.
[26] In patients with symptoms typical of myocardial ischemia an electrocardiogram must be immediately obtained - e.g., within 10 minutes from first contact with medical or paramedical personnel, including prehospital setting; the electrocardiographic findings will guide the subsequent management.
Serum cardiac biomarkers are routinely obtained and their elevation is necessary for confirming diagnosis of myocardial infarction;[27] however, reperfusion must not be delayed by waiting for the results.
They must also be avoided in patients who have taken sildenafil or other phosphodiesterase type 5 inhibitors (used for erectile dysfunction) within the previous 24–48 hours, as the combination of the two could cause a serious drop in blood pressure.
Beta-blockers alleviate ischemic pain, and have also been proved to reduce the size of infarcted heart muscle, the risk of arrhythmias, and the proportion of patients with acute coronary syndrome who actually evolve STEMI.
[31][38][39] However, in patients presenting without ST elevation, morphine has been shown to have adverse events potential, and its use is considered acceptable only after inadequate pain relief by medication specific against angina.
[45][46] Glycoprotein IIb/IIIa inhibitors are a class of intravenous antiplatelet agents used in patients undergoing percutaneous coronary intervention, consisting of abciximab, eptifibatide and tirofiban.
Administering eptifibatide or tirofiban may also be reasonable in patients presenting with NST-ACS who are considered of intermediate or high risk and are treated with early invasive strategy.
Unfractionated heparin has the disadvantage of requiring dose adjustment based on a laboratory exam, activated partial thromboplastin time (APTT).
[53][54] Patients who present with suspected acute myocardial infarction and ST segment elevation (STEMI) or new bundle branch block on the 12 lead ECG are presumed to have an occlusive thrombosis in an epicardial coronary artery.
[55] The basis for this distinction in treatment regimens is that ST segment elevations on an ECG are typically due to complete occlusion of a coronary artery.
[citation needed] At least 10% of patients with STEMI do not develop myocardial necrosis (as evidenced by a rise in cardiac markers) and subsequent Q waves on EKG after reperfusion therapy.
[60] Physical exercise is an important part of rehabilitation after a myocardial infarction, with beneficial effects on cholesterol levels, blood pressure, weight, stress and mood.
[64] Cocaine associated myocardial infarction should be managed in a manner similar to other patients with acute coronary syndrome, except that beta blockers should not be used and benzodiazepines should be administered early.
The suspicion or provisional diagnosis of an MI means that it is inappropriate for the patient to walk out of the wilderness setting and will require them to be carried or conveyed in a vehicle.
Aspirin, nitroglycerin, and oxygen can all be given with relative ease in a wilderness setting and should be administered as soon as possible in suspected cases of MI.
Wilderness management of cardiac arrest differs slightly from that carried out in an urban setting in that it is generally considered acceptable to terminate a resuscitation attempt after 30 minutes if there has been no change in the patient's condition.
[citation needed] Certified personnel traveling by commercial aircraft may be able to assist an MI patient by using the on-board first aid kit, which may contain some cardiac drugs (such as glyceryl trinitrate spray, aspirin, or opioid painkillers), an AED,[67] and oxygen.