Osteopathic medicine in the United States
[4] Osteopathic physicians attend four years of medical school like their MD counterparts, acquiring equivalent education in medicine and surgery; DOs also attend the same graduate medical education programs (ACGME-accredited residencies and fellowships) as their MD counterparts to acquire their licenses as physicians.
Those holding the DO degree are commonly referred to as "osteopathic physicians", and they learn, train in, and practice the full scope of mainstream evidence-based medicine and surgery.
[23] The states with the lowest concentrations of DOs are Washington, D.C., North Dakota, and Vermont, where only 1–3% of physicians have an osteopathic medical degree.[when?
[27] In the Northeastern United States, osteopathic physicians provided more than one-third of general and family medicine patient visits between 2003 and 2004.
Revised in 1953, and again in 2002, the core principles are: Contemporary osteopathic physicians practice evidence-based medicine, indistinguishable from their MD colleagues.
Still believed that the conventional medical system lacked credible efficacy, was morally corrupt and treated effects rather than causes of disease.
[32][33] He founded osteopathic medicine in rural Missouri at a time when medications, surgery, and other traditional therapeutic regimens often caused more harm than good.
He invented the name "osteopathy" by blending two Greek roots osteon- for bone and -pathos for suffering to communicate his theory that disease and physiologic dysfunction were etiologically grounded in a disordered musculoskeletal system.
[38] Recognition by the US federal government was a key goal of the osteopathic medical profession in its effort to establish equivalency with its MD counterparts.
On May 3, 1966 Secretary of Defense Robert McNamara authorized the acceptance of osteopathic physicians into all the medical military services on the same basis as MDs.
"By attending a short seminar and paying $65, a doctor of osteopathy (DO) could obtain an MD degree; 86 percent of the DOs in the state (out of a total of about 2000) chose to do so.
Today, a majority of osteopathic physicians are trained alongside MDs, in residency programs governed by the ACGME, an independent board of the AMA.
[54] Within the osteopathic medical curriculum, manipulative treatment is taught as an adjunctive measure to other biomedical interventions for several disorders and diseases.
He describes problems with "the quality, breadth, nature, and orientation of OMM instruction," and he claims that the teaching of osteopathic medicine has not changed sufficiently over the years to meet the intellectual and practical needs of students.
Even worse, faculty members rarely provide instrument-based objective evidence that somatic dysfunction is present in the first place.
studies show an increasingly positive attitude of patients and physicians (MD and DO) toward the use of manual therapy as a valid, safe, and effective treatment modality.
[57] Another small study examined the interest and ability of MD residents in learning osteopathic principles and skills, including OMT.
In 2005, during his tenure as president of the Association of American Medical Colleges, Jordan Cohen described a climate of cooperation between DO and MD practitioners: "We now find ourselves living at a time when osteopathic and allopathic graduates are both sought after by many of the same residency programs; are in most instances both licensed by the same licensing boards; are both privileged by many of the same hospitals; and are found in appreciable numbers on the faculties of each other's medical schools".
The BIOMEA monitors the licensing and registration practices of physicians in countries outside of the United States and advances the recognition of American-trained DOs.
The American Osteopathic Association has lobbied the governments of other countries to recognize US-trained DOs similarly to their MD counterparts, with some success.
"[63] The American Medical Student Association strongly advocates for US-trained DO international practice rights "equal to that" of MD-qualified physicians.
The acknowledgment draws a clear separation between American DOs, who are medical doctors, and non-physician osteopaths trained outside of the United States.
degree, e.g. the Association of Medical Councils of Africa (AMCOA) approved a resolution in 2019 granting the AOA's request that AMCOA recognizes U.S.-trained DOs as fully licensed physicians with practice rights equivalent to MDs, opening its 20 member countries, which include Botswana, Gambia, Ghana, Kenya, Lesotho, Liberia, Malawi, Mauritius, Namibia, Nigeria, Rwanda, Seychelles, Sierra Leone, South Africa, South Sudan, Swaziland, Tanzania, Uganda, Zambia, and Zimbabwe to DO's.
[citation needed] Osteopathic physicians have historically entered primary care fields at a higher rate than their MD counterparts.
[67] Medical research has found no good evidence that either CST or cranial osteopathy confers any health benefit, and they can be harmful, particularly if used on children or infants.
[68][69][70] The basic assumptions of CST are challenged by some medical doctors, and practitioners produce conflicting and mutually exclusive diagnoses of the same patients.
[83][84] Howell summarizes the questions framing the debate over the future of osteopathic distinctiveness thus: If osteopathy has become the functional equivalent of allopathy [meaning the MD profession], what is the justification for its continued existence?
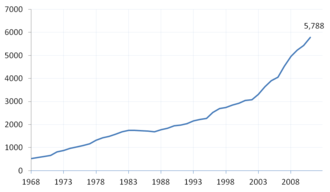
Norman Gevitz, author of the leading text on the history of osteopathic medicine, wrote in 2009, DO schools are currently expanding their class sizes much more quickly than are their MD counterparts.
Osteopathic medical schools can keep the cost of student body expansion relatively low compared with that of MD institutions.
The simultaneous movement away from osteopathic medicine’s traditionally separate training and practice systems, when coupled with its rapid growth, has created a sense of crisis as to its future.







1901–1930 1931–1966 1967–1989