Oxygen toxicity
These protocols have resulted in the increasing rarity of seizures due to oxygen toxicity, with pulmonary and ocular damage being largely confined to the problems of managing premature infants.
[2][15] In unusual circumstances, effects on other tissues may be observed: it is suspected that during spaceflight, high oxygen concentrations may contribute to bone damage.
[16] Hyperoxia can also indirectly cause carbon dioxide narcosis in patients with lung ailments such as chronic obstructive pulmonary disease or with central respiratory depression.
[18][20][21] In addition, many external factors, such as underwater immersion, exposure to cold, and exercise will decrease the time to onset of central nervous system symptoms.
[40] CNS toxicity is aggravated by a high partial pressure of carbon dioxide, stress, fatigue, and cold, all of which are much more likely in diving than in hyperbaric therapy.
[28] The lungs and the remainder of the respiratory tract are exposed to the highest concentration of oxygen in the human body and are therefore the first organs to show chronic toxicity.
[47][54] A possible side effect of hyperbaric oxygen therapy is the initial or further development of cataracts, which are an increase in opacity of the lens of the eye which reduces visual acuity, and can eventually result in blindness.
This is a rare event, associated with lifetime exposure to raised oxygen concentration, and may be under-reported as it develops very slowly, and cataracts are a common disorder of advanced age.
[63] High concentrations of oxygen also increase the formation of other free radicals, such as nitric oxide, peroxynitrite, and trioxidane, which harm DNA and other biomolecules.
[68] Diagnosis of central nervous system oxygen toxicity in divers prior to seizure is difficult as the symptoms of visual disturbance, ear problems, dizziness, confusion and nausea can be due to many factors common to the underwater environment such as narcosis, congestion and coldness.
Prematurity, low birth weight, and a history of oxygen exposure are the principal indicators, while no hereditary factors have been shown to yield a pattern.
In this case prevention of bronchopulmonary dysplasia and retinopathy of prematurity must be carried out without compromising a supply of oxygen adequate to preserve the infant's life.
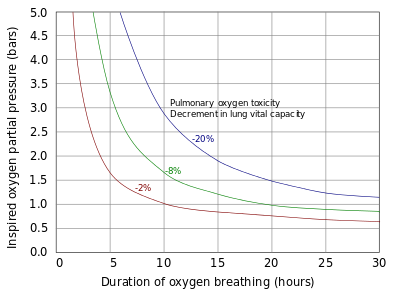
The risk to a specific person can vary considerably depending on individual sensitivity, level of exercise, and carbon dioxide retention, which is influenced by work of breathing.
[76] This is a notional alarm clock, which ticks more quickly at increased oxygen pressure and is set to activate at the maximum single exposure limit recommended in the National Oceanic and Atmospheric Administration Diving Manual.
[97] Bronchopulmonary dysplasia is reversible in the early stages by use of break periods on lower pressures of oxygen, but it may eventually result in irreversible lung injury if allowed to progress to severe damage.
Although for many years the recommendation has been not to raise the diver during the seizure itself, owing to the danger of arterial gas embolism (AGE),[101] there is some evidence that the glottis does not fully obstruct the airway.
[103] If symptoms develop other than a seizure underwater the diver should immediately switch to a gas with a lower oxygen fraction or ascend to a shallower depth if decompression obligations allow.
An overview of these studies by Bitterman in 2004 concluded that following removal of breathing gas containing high fractions of oxygen, no long-term neurological damage from the seizure remains.
[38] The incidence of central nervous system toxicity among divers has decreased since the Second World War, as protocols have developed to limit exposure and partial pressure of oxygen inspired.
Careful titration of oxygen supply to minimise the excess to physiological need also reduces pulmonary hyperoxic exposure to the reasonably practicable minimum.
[119][120] He showed that oxygen was toxic to insects, arachnids, myriapods, molluscs, earthworms, fungi, germinating seeds, birds, and other animals.
[3] Smith then went on to show that intermittent exposure to a breathing gas with less oxygen permitted the lungs to recover and delayed the onset of pulmonary toxicity.
[124][125] In the decade following World War II, Lambertsen et al. made further discoveries on the effects of breathing oxygen under pressure and methods of prevention.
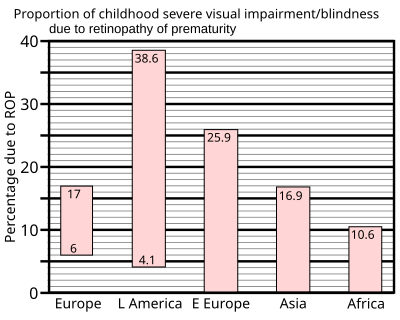
[23][24][129] Retinopathy of prematurity was not observed before World War II, but with the availability of supplemental oxygen in the decade following, it rapidly became one of the principal causes of infant blindness in developed countries.
Since then, more sophisticated monitoring and diagnosis have established protocols for oxygen use which aim to balance between hypoxic conditions and problems of retinopathy of prematurity.
[133] Sensitivity to central nervous system oxygen toxicity has been shown to be affected by factors such as circadian rhythm, drugs, age, and gender.
[134][135][136][137] In 1988, Hamilton et al. wrote procedures for the National Oceanic and Atmospheric Administration to establish oxygen exposure limits for habitat operations.
Claims have been made that this reduces stress, increases energy, and lessens the effects of hangovers and headaches, despite the lack of any scientific evidence to support them.
In "Dr. Ox's Experiment", a short story written by Jules Verne in 1872, the eponymous doctor uses electrolysis of water to separate oxygen and hydrogen.
He then pumps the pure oxygen throughout the town of Quiquendone, causing the normally tranquil inhabitants and their animals to become aggressive and plants to grow rapidly.