Patient safety
People did not recognize the magnitude of avoidable adverse events until the 1990s, when several countries reported alarming numbers of patients harmed and killed by medical errors.
There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety,[3] with mobile health apps becoming an increasingly important area of study.
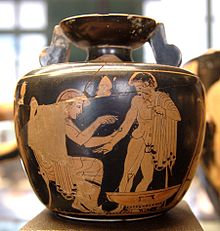
Greek healers in the 4th century BC drafted the Hippocratic Oath and pledged to "prescribe regimens for the good of my patients according to my ability and my judgment and never do harm to anyone.
However, despite an increasing emphasis on the scientific basis of medical practice in Europe and the United States in the late 19th century, data on adverse outcomes were hard to come by, and the various studies commissioned collected mostly anecdotal events.
[7] In 1983, the British Royal Society of Medicine and the Harvard Medical School jointly sponsored a symposium on anesthesia deaths and injuries, resulting in an agreement to share statistics and conduct studies.
[citation needed] In the United States, the full magnitude and impact of errors in health care were not appreciated until the 1990s, when several reports brought attention to this issue.
[15] Initial criticisms of the methodology in the IOM estimates[16] focused on the statistical methods of amplifying low numbers of incidents in the pilot studies to the general population.
One significant influence on this is nurse burnout, leading to hundreds of thousands of deaths a year and billions of dollars spent when having to rectify a new problem; this is a real issue in the world.
Freudenberger was working at a free clinic, and over time mentioned some of the effects that he had seen, such as "emotional depletion and accompanying psychosomatic symptoms... excessive demands on energy, strength, or resources".
However, hospitals pay both higher costs for implementation and potentially lower revenues (depending on reimbursement scheme) due to reduced patient length of stay.
[92] These systems' basic security measures are based on sound identifying electronic tags, in order that the patient details provided in different situations are always reliable.
The clinician uses pertinent clinical research on the accuracy of diagnostic tests and the efficacy and safety of therapy, rehabilitation, and prevention to develop an individual plan of care.
[107] Advantages:[108][109] Drawbacks:[110][111] Community pharmacy practice is making important advances in the quality and safety movement despite the limited number of federal and state regulations that exist and in the absence of national accreditation organizations such as the Joint Commission - a driving force for performance improvement in health care systems.
The goal of AHRQ is to refine the area-level indicators to improve outcomes for children receiving outpatient care and reduce the incidence of hospitalization for those defined conditions.
Studies by Aiken and Needleman have demonstrated that patient death, nosocomial infections, cardiac arrest, and pressure ulcers are linked to inadequate nurse-to-patient ratios.
[123][124] The presence or absence of registered nurses (RNs) impacts the outcome for pediatric patients requiring pain management and/or peripheral administration of intravenous fluids and/or medications.
Astute assessment skills are required to intervene successfully and relieve discomfort.33 Maintenance of a patient's intravenous access is a clear nursing responsibility.
As of 2005[update], 75 percent of all U.S. companies connected at least part of an employee's pay to measures of performance, and in healthcare, over 100 private and federal pilot programs were underway.
Methods of healthcare payment current at that time may actually have rewarded less-safe care, since some insurance companies will not pay for new practices to reduce errors, while physicians and hospitals can bill for additional services that are needed when patients are injured by mistakes.
[138] However, early studies showed little gain in quality for the money spent,[139][140] as well as evidence suggesting unintended consequences, like the avoidance of high-risk patients, when payment was linked to outcome improvements.
[151] In the United States, Medicare has various pay-for-performance ("P4P") initiatives in offices, clinics, and hospitals, seeking to improve quality and avoid unnecessary healthcare costs.
However, pilot programs now underway focus on simple indicators such as improvement in lab values or use of emergency services, avoiding areas of complexity such as multiple complications or several treating specialists.
[166] Patients with low health literacy, inadequate financial resources to afford expensive medications or treatments, and ethnic groups traditionally subject to healthcare inequities may also be deselected by providers seeking improved performance measures.
[168] The Danish Act on Patient Safety[169] passed Parliament in June 2003, and on January 1, 2004, Denmark became the first country to introduce nationwide mandatory reporting.
"[172] Professional organizations, such as the Anesthesia Patient Safety Foundation, responded negatively: "Mandatory reporting systems, in general, create incentives for individuals and institutions to play a numbers game.
[184][185] However, many doctors and hospitals do not report errors under the current system because of concerns about malpractice lawsuits; this prevents collection of information needed to find and correct the conditions that lead to mistakes.
Numerous organizations, government branches, and private companies conduct research studies to investigate the overall health of patient safety in America and across the globe.
Despite the shocking and widely publicized statistics on preventable deaths due to medical errors in America's hospitals, the 2006 National Healthcare Quality Report[198] assembled by the Agency for Healthcare Research and Quality (AHRQ) had the following sobering assessment:A 2011 study of more than 1,000 patients with advanced colon cancer found that one in eight were treated with at least one drug regimen with specific recommendations against its use in the National Comprehensive Cancer Network guidelines.
[199] Several authors of the 1999 Institute of Medicine report revisited the status of their recommendations and the state of patient safety, five years after "To Err is Human".
[138] Discovering that patient safety had become a frequent topic for journalists, health care experts, and the public, it was harder to see overall improvements on a national level.