Pharmacogenomics
[2][3][4] Pharmacogenomics aims to develop rational means to optimize drug therapy, with regard to the patients' genotype, to achieve maximum efficiency with minimal adverse effects.
In order to provide pharmacogenomic recommendations for a given drug, two possible types of input can be used: genotyping, or exome or whole genome sequencing.
[10] Sequencing provides many more data points, including detection of mutations that prematurely terminate the synthesized protein (early stop codon).
An increase, decrease, or loss of function for transporters or metabolizing enzymes can ultimately alter the amount of medication in the body and at the site of action.
One well-established gene-drug interaction involving a germline mutation to a drug target is warfarin (Coumadin) and VKORC1, which codes for vitamin K epoxide reductase (VKOR).
When medications that have a significant oxidative effect are administered to individuals who are G6PD deficient, they are at an increased risk of erythrocyte lysis that presents as hemolytic anemia.
[24] For the gene-drug pairs included in the table, "the FDA has evaluated and believes there is sufficient scientific evidence to suggest that subgroups of patients with certain genetic variants, or genetic variant-inferred phenotypes (such as affected subgroup in the table below), are likely to have altered drug metabolism, and in certain cases, differential therapeutic effects, including differences in risks of adverse events.
"Biomarkers in the table include but are not limited to germline or somatic gene variants (polymorphisms, mutations), functional deficiencies with a genetic etiology, gene expression differences, and chromosomal abnormalities; selected protein biomarkers that are used to select treatments for patients are also included.
"[26] The Pharmacogenomics Knowledgebase (PharmGKB) is an "NIH-funded resource that provides information about how human genetic variation affects response to medications.
In behavioral health, pharmacogenomic tests provide tools for physicians and care givers to better manage medication selection and side effect amelioration.
Beside efficacy, germline pharmacogenetics can help to identify patients likely to undergo severe toxicities when given cytotoxics showing impaired detoxification in relation with genetic polymorphism, such as canonical 5-FU.
[32] In particular, genetic deregulations affecting genes coding for DPD, UGT1A1, TPMT, CDA and CYP2D6 are now considered as critical issues for patients treated with 5-FU/capecitabine, irinotecan, mercaptopurine/azathioprine, gemcitabine/capecitabine/AraC and tamoxifen, respectively.
[33] In cardiovascular disorders, the main concern is response to drugs including warfarin, clopidogrel, beta blockers, and statins.
[10] In patients with CYP2C19, who take clopidogrel, cardiovascular risk is elevated, leading to medication package insert updates by regulators.
[36] Initiatives to spur adoption by clinicians include the Ubiquitous Pharmacogenomics (U-PGx) program in Europe and the Clinical Pharmacogenetics Implementation Consortium (CPIC) in the United States.
[38] In 2010, Vanderbilt University Medical Center launched Pharmacogenomic Resource for Enhanced Decisions in Care and Treatment (PREDICT);[39] in 2015 survey, two-thirds of the clinicians had ordered a pharmacogenetic test.
[40] In 2019, the largest private health insurer, UnitedHealthcare, announced that it would pay for genetic testing to predict response to psychiatric drugs.
[42] A potential role for pharmacogenomics is to reduce the occurrence of polypharmacy: it is theorized that with tailored drug treatments, patients will not need to take several medications to treat the same condition.
Thus they could potentially reduce the occurrence of adverse drug reactions, improve treatment outcomes, and save costs by avoiding purchase of some medications.
[43] The need for pharmacogenomically tailored drug therapies may be most evident in a survey conducted by the Slone Epidemiology Center at Boston University from February 1998 to April 2007.
Although the patient lost the excessive weight they had gained, they then developed muscle stiffness, cogwheeling, tremors and night sweats.
Over the course of 8 months, patient A gradually experienced more weight gain and sedation, and developed difficulty with their gait, stiffness, cogwheeling and dyskinetic ocular movements.
It is assumed that if the patient had undergone a pharmacogenomic test, it would have revealed she may have had a duplication of the gene CYP2D6, placing her in the Ultra-rapid metabolizer (UM) category, explaining her reactions to codeine use.
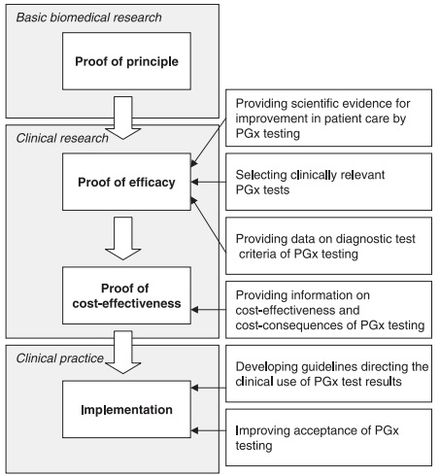
Increasingly substantial evidence and industry body guidelines for clinical use of pharmacogenetics have made it a population wide approach to precision medicine.
[54] In the early 2000s, handling genetic information as exceptional, including legal or regulatory protections, garnered strong support.
It was argued that genomic information may need special policy and practice protections within the context of electronic health records (EHRs).
[60] Genomic contextualism would allow for a case-by-case analysis of the technology and the context of its use (e.g., clinical practice, research, secondary findings).
[63] Pharmacogenomics was first recognized by Pythagoras around 510 BC when he made a connection between the dangers of fava bean ingestion with hemolytic anemia and oxidative stress.
[72] Technology now allows for genetic analysis of hundreds of target genes involved in medication metabolism and response in less than 24 hours for under $1,000.
The companies use the same genotyping chips that are used in GWAS studies and provide customers with a write-up of individual risk for various traits and diseases and testing for 500,000 known SNPs.