Pre-exposure prophylaxis for HIV prevention
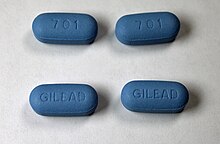
[3] In October 2019, the U.S. Food and Drug Administration (FDA) approved the combination of emtricitabine and tenofovir alafenamide (FTC/TAF; Descovy) to be used as PrEP in addition to Truvada, which provides similar levels of protection.
[4] Descovy, however, is currently approved only for cisgender males and transgender women as the efficacy has not been assessed in people at risk for HIV through receptive vaginal sex.
Regulators believe it will improve medication adherence because it has to be taken just once every two months, and it will also widen adoption as it eliminates the need to hide pills or pharmacy visits for discretion.
[11][2] Effectiveness of PrEP is associated with adherence, meaning the more consistently a person takes the medication as prescribed the greater the chance at reducing their risk for HIV.
[9] Studies evaluating PrEP efficacy to reduce risk of HIV infection found a linear relationship between adherence and effectiveness of medication.
[17] This dosing regimen was first proven effective to reduce the relative risk of HIV infection by 86% in the IPERGAY randomized clinical trial performed in Canada and France in 2015.
[19] The World Health Organization (WHO) recommendations support the use of PrEP in pregnant and breastfeeding people who are at substantial risk of HIV infection.
[23][24] Research shows that pre-exposure prophylaxis (PrEP) is generally safe and well tolerated for most individuals, although some side effects have been noted to occur.
[2][9][25] Research has shown that the use of Truvada has been associated with mild to moderate declines in kidney function, mostly associated with older people over 50, those with predisposing conditions such as diabetes, or glomerular filtration rate lower than 90.
Research and study outcome analysis suggests that emtricitabine/tenofovir does not have a significant effect on fat redistribution or accumulation when used as pre-exposure prophylaxis in HIV negative individuals.
[38] Other potential serious side effects of Truvada include acute exacerbations of hepatitis B in individuals with HBV infection, lactic acidosis, and severe hepatomegaly with steatosis.
Cabotegravir (Apretude) shares a similar black box warning to only use the medication if a person tests negative for HIV infection.
The WHO noted that "international scientific consensus is emerging that antiretroviral drugs, including PrEP, significantly reduce the risk of sexual acquisition and transmission of HIV regardless of population or setting.
"[43]: 4 In November 2015 the WHO expanded this further, on the basis of further evidence, and stated that it had "broadened the recommendation to include all population groups at substantial risk of HIV infection" and emphasized that PrEP should be "an additional prevention choice in a comprehensive package of services.
Funded access to PrEP will require that people undergo regular testing for HIV and other sexually transmitted infections, and are monitored for risk of side effects.
People taking funded PrEP will receive advice on ways to reduce the risk of HIV and sexually transmitted infections.
[52] In Australia, the country's Therapeutic Goods Administration approved the use of Truvada as PrEP in May 2016, allowing Australian providers to legally prescribe the medication.
On March 21, 2018, the Federal Minister for Health announced that PrEP will be subsidized by the Australian Government through the Pharmaceutical Benefits Scheme (PBS) from April 1, 2018.
The Global Fund to Fight AIDS, Tuberculosis and Malaria, stated that the goal is to begin distributing Gilead Sciences’ lenacapavir within that timeframe.
[55] Already approved as a treatment for multi-drug resistant HIV—costing approximately $42,250 for the first year in the U.S.—lenacapavir has also shown strong efficacy in preventing HIV infection during recent clinical trials.
Expected fall of 2020, Teva Pharmaceuticals will begin producing a generic version of Truvada within the United States; however, it has been reported that the details surrounding the rights to the patent are unclear, which makes it difficult to predict if this will increase access to the medications.
[66] The law is recognized by pharmacist organizations, health providers, legislators, and the general public to be the removal of a barrier to direct and time-dependent access to these medications, especially for those in communities most affected by HIV/AIDs.
The campaign aims to dramatically reduce the number of new HIV infections in the city and relies on expanding access to PrEP as a key strategy for achieving that goal.
For example, the U.K.'s NHS initially refused to offer PrEP to individuals citing concerns about cost and suggested that local officials ought to bear the responsibility of paying for the drug.
[95] Additional barriers transgender women face include concerns about side effects, hormone therapy, adherence, and interaction with healthcare workers.
[96] Challenges encountered by people engaging in injection drug use include limited access to healthcare providers, expense of medication, and follow-up for HIV testing.
Initial studies of PrEP strategies in non-human primates showed a reduced risk of infection among animals that receive ARVs prior to exposure to a simian form of HIV.
[medical citation needed] A 2007 study at UT-Southwestern (Dallas) and the University of Minnesota showed PrEP to be effective in "humanized" laboratory mice.
[102] Similarly, researchers are investigating whether drugs could be used in ways other than a daily pill to prevent HIV, including PrEP-releasing implants or rectally administered PrEP.
[22] At the 2024 International AIDS Conference, PrEP with long-acting injectable cabotegravir (CAB-LA; Apretude) appears safe during pregnancy among cisgender women, according to an analysis from the HPTN 084 open-label extension trial.


|
Approved
Under review
Not approved
No data
|
