Psychiatry
Research within psychiatry is conducted on an interdisciplinary basis with other professionals, such as epidemiologists, nurses, social workers, occupational therapists, and clinical psychologists.
"Psychiatry, more than any other branch of medicine, forces its practitioners to wrestle with the nature of evidence, the validity of introspection, problems in communication, and other long-standing philosophical issues" (Guze, 1992, p.4).
Psychiatry refers to a field of medicine focused specifically on the mind, aiming to study, prevent, and treat mental disorders in humans.
In establishing such ethical codes, the profession has responded to a number of controversies about the practice of psychiatry, for example, surrounding the use of lobotomy and electroconvulsive therapy.
Discredited psychiatrists who operated outside the norms of medical ethics include Harry Bailey, Donald Ewen Cameron, Samuel A. Cartwright, Henry Cotton, and Andrei Snezhnevsky.
Mental illness can be assessed, conversely, through a narrative which tries to incorporate symptoms into a meaningful life history and to frame them as responses to external conditions.
Both approaches are important in the field of psychiatry[27] but have not sufficiently reconciled to settle controversy over either the selection of a psychiatric paradigm or the specification of psychopathology.
[28] Alternatively, a Niall McLaren acknowledges the physiological basis for the mind's existence but identifies cognition as an irreducible and independent realm in which disorder may occur.
[28][29][30] The biocognitive approach includes a mentalist etiology and provides a natural dualist (i.e., non-spiritual) revision of the biopsychosocial view, reflecting the efforts of Australian psychiatrist Niall McLaren to bring the discipline into scientific maturity in accordance with the paradigmatic standards of philosopher Thomas Kuhn.
[31] Behaviorism is a therapeutic school of thought that elects to focus solely on real and observable events, rather than mining the unconscious or subconscious.
[34] Strategies to address this shortfall have included the use of short 'taster' placements early in the medical school curriculum[33] and attempts to extend psychiatry services further using telemedicine technologies and other methods.
Forensic psychiatry utilizes medical science generally, and psychiatric knowledge and assessment methods in particular, to help answer legal questions.
[17][50][51][52] Under the supervision of institutional review boards, psychiatric clinical researchers look at topics such as neuroimaging, genetics, and psychopharmacology in order to enhance diagnostic validity and reliability, to discover new treatment methods, and to classify new mental disorders.
[67] The stated intention of diagnostic manuals is typically to develop replicable and clinically useful categories and criteria, to facilitate consensus and agreed upon standards, whilst being atheoretical as regards etiology.
There are ongoing issues concerning the validity and reliability of the diagnostic categories; the reliance on superficial symptoms; the use of artificial dividing lines between categories and from 'normality'; possible cultural bias; medicalization of human distress and financial conflicts of interest, including with the practice of psychiatrists and with the pharmaceutical industry; political controversies about the inclusion or exclusion of diagnoses from the manual, in general or in regard to specific issues; and the experience of those who are most directly affected by the manual by being diagnosed, including the consumer/survivor movement.
Alternatively, a person may be referred by hospital medical staff, by court order, involuntary commitment, or, in countries such as the UK and Australia, by sectioning under a mental health law.
The Italian movement, heavily influenced by Franco Basaglia, emphasizes ethical treatment and the elimination of physical restraints in psychiatric care.
A study examining the application of these principles in Italy found that 14 general hospital psychiatric units reported zero restraint incidents in 2022.
[87] A major reason for this change was the advent of managed care insurance plans,[clarification needed] which began to limit reimbursement for psychotherapy sessions provided by psychiatrists.
[88][89][90][91][a][excessive citations] Because of this shift in practice patterns, psychiatrists often refer patients whom they think would benefit from psychotherapy to other mental health professionals, e.g., clinical social workers and psychologists.
[101] During the 5th century BCE, mental disorders, especially those with psychotic traits, were considered supernatural in origin,[102] a view which existed throughout ancient Greece and Rome,[102] as well as Egyptian regions.
[108] An ancient text known as The Yellow Emperor's Classic of Internal Medicine identifies the brain as the nexus of wisdom and sensation, includes theories of personality based on yin–yang balance, and analyzes mental disorder in terms of physiological and social disequilibria.
Chinese scholarship that focused on the brain advanced during the Qing Dynasty with the work of Western-educated Fang Yizhi (1611–1671), Liu Zhi (1660–1730), and Wang Qingren (1768–1831).
[110] In 1656, Louis XIV of France created a public system of hospitals for those with mental disorders, but as in England, no real treatment was applied.
Battie argued for a tailored management of patients entailing cleanliness, good food, fresh air, and distraction from friends and family.
Patients were allowed to move freely about the hospital grounds, and eventually dark dungeons were replaced with sunny, well-ventilated rooms.
At the Lincoln Asylum in England, Robert Gardiner Hill, with the support of Edward Parker Charlesworth, pioneered a mode of treatment that suited "all types" of patients, so that mechanical restraints and coercion could be dispensed with—a situation he finally achieved in 1838.
[115][116][page needed] The modern era of institutionalized provision for the care of the mentally ill, began in the early 19th century with a large state-led effort.
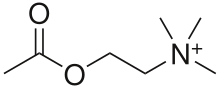
Psychopharmacology and neurochemistry became the integral parts of psychiatry starting with Otto Loewi's discovery of the neuromodulatory properties of acetylcholine; thus identifying it as the first-known neurotransmitter.
Rashed argues new mental health science has moved beyond this reductionist critique by seeking integrative and biopsychosocial models for conditions and that much of critical psychiatry now exists with orthodox psychiatry but notes that many critiques remain unaddressed[132]: 237 The term anti-psychiatry was coined by psychiatrist David Cooper in 1967 and was later made popular by Thomas Szasz.