Staphylococcus epidermidis
[4] S. epidermidis is a particular concern for people with catheters or other surgical implants because it is known to form biofilms that grow on these devices.
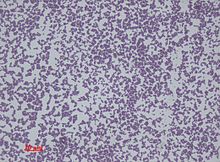
Staphylococcus epidermidis is a very hardy microorganism, consisting of nonmotile, Gram-positive cocci, arranged in grape-like clusters.
It forms white, raised, cohesive colonies about 1–2 mm in diameter after overnight incubation, and is not hemolytic on blood agar.
[12][13] It is sensitive to novobiocin, providing an important test to distinguish it from Staphylococcus saprophyticus, which is coagulase-negative, as well, but novobiocin-resistant.
[4] Similar to those of S. aureus, the cell walls of S. epidermidis have a transferrin-binding protein that helps the organism obtain iron from transferrin.
The tetramers of a surface exposed protein, glyceraldehyde-3-phosphate dehydrogenase, are believed to bind to transferrin and remove its iron.
Increasingly, techniques such as quantitative PCR are being employed for the rapid detection and identification of Staphylococcus strains.
[17] S. epidermidis thrives in warm, moist environments and is a common bacteria of the human microbiome;[18] it is thus primarily responsible for foot odor as feet have more sweat glands than any other part of the body and thus are often moist, which creates an ideal environment for S. epidermidis to thrive.
[citation needed] The ability to form biofilms on plastic devices is a major virulence factor for S. epidermidis.
S. epidermidis strains are often resistant to antibiotics, including rifamycin, fluoroquinolones, gentamicin, tetracycline, clindamycin, and sulfonamides.
Staphylococcus epidermidis enters the sebaceous gland (colonized by Cutibacterium acnes, the main bacterium that causes acne vulgaris) and damages the hair follicles by producing lipolytic enzymes that change the sebum from fraction to dense (thick) form leading to inflammatory effect.
[22] Moreover, S. epidermidis biofilm formation by releasing the exopolysaccharide intercellular adhesion (PIA) provides the susceptible anaerobic environment to P. acnes colonisation and protects it from the innate human immunity molecules.
But in the case of competition, they use the same carbon source (i.e. glycerol) to produce short chain fatty acids which act as antibacterial agent against each other.
By modulating the moist, inner lining of some organs and body cavities and their specific immune defense mechanisms, skin commensals interact with infectious agents like pathogens.
Sphingomyelin phosphodiesterase is the main driver in the S. epidermidis production of ceramides - a lipid that includes sphingosine and sphingosine-1-phosphate.
[25] In the case of S. aureus, S. epidermidis may amplify the innate immune response by causing a reaction of keratinocytes toward this pathogen.
These immunomodulatory molecules create a relationship between bacteria and keratinocytes and have a significant impact in the modulation of the innate immune response, mainly because of their interactions with TLRs.