Hemodialysis
Routine hemodialysis is conducted in a dialysis outpatient facility, either a purpose-built room in a hospital or a dedicated, stand-alone clinic.
[3] Unfractioned heparin (UHF) is the most commonly used anticoagulant in hemodialysis, as it is generally well tolerated and can be quickly reversed with protamine sulfate.
[4] Compared to UHF, LMWH has the advantage of an easier mode of administration and reduced bleeding but the effect cannot be easily reversed.
For example, in 2008, a series of first-use type of reactions, including deaths, occurred due to heparin contaminated during the manufacturing process with oversulfated chondroitin sulfate.
Increasing the frequency and length of treatments has been shown to improve fluid overload and enlargement of the heart that is commonly seen in such patients.
If a high concentration of sodium is added to the dialysate, the patient can become thirsty and end up accumulating body fluids, which can lead to heart damage.
Three primary methods are used to gain access to the blood for hemodialysis: an intravenous catheter, an arteriovenous fistula (AV) and a synthetic graft.
[16] The newest dialysis machines on the market are highly computerized and continuously monitor an array of safety-critical parameters, including blood (QB) and dialysate QD) flow rates;[17] dialysis solution conductivity, temperature, and pH; and analysis of the dialysate for evidence of blood leakage or presence of air.
[18] Manufacturers of dialysis machines include companies such as Nipro, Fresenius, Gambro, Baxter, B. Braun, NxStage and Bellco.
Because the damaged kidneys cannot perform their intended function of removing impurities, molecules introduced into the bloodstream from improperly purified water can build up to hazardous levels, causing numerous symptoms or death.
Aluminum, chlorine and or chloramines, fluoride, copper, and zinc, as well as bacterial fragments and endotoxins, have all caused problems in this regard.
The trend lately is to pass this final purified water (after mixing with dialysate concentrate) through an ultrafiltration membrane or absolute filter.
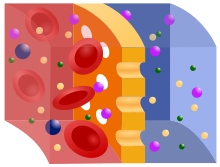
A cylindrical bundle of hollow fibers, whose walls are composed of semi-permeable membrane, is anchored at each end into potting compound (a sort of glue).
The NIH-funded HEMO trial compared survival and hospitalizations in patients randomized to dialysis with either low-flux or high-flux membranes.
High-flux dialysis membranes and/or intermittent internal on-line hemodiafiltration (iHDF) may also be beneficial in reducing complications of beta-2-microglobulin accumulation.
After several years (usually at least 5–7), patients on hemodialysis begin to develop complications from beta-2-M accumulation, including carpal tunnel syndrome, bone cysts, and deposits of this amyloid in joints and other tissues.
Single used dialyzers are initiated just once and then thrown out creating a large amount of bio-medical waste with no mercy for cost savings.
The dialyzer is first pre-cleaned by a technician, then automatically cleaned by machine through a step-cycles process until it is eventually filled with liquid disinfectant for storage.
When reused over 15 times with current methodology, the dialyzer can lose B2m, middle molecule clearance and fiber pore structure integrity, which has the potential to reduce the effectiveness of the patient's dialysis session.
[32] As medical reimbursement rates begin to fall even more, many dialysis clinics are continuing to operate effectively with reuse programs especially since the process is easier and more streamlined than before.
[33] Many have played a role in developing dialysis as a practical treatment for renal failure, starting with Thomas Graham of Glasgow, who first presented the principles of solute transport across a semipermeable membrane in 1854.
Kolff gave a set of blueprints for his hemodialysis machine to George Thorn at the Peter Bent Brigham Hospital in Boston.
According to McKellar (1999), a significant contribution to renal therapies was made by Canadian surgeon Gordon Murray with the assistance of two doctors, an undergraduate chemistry student, and research staff.
The less-crude, more compact, second-generation "Murray-Roschlau" dialyser was invented in 1952–53, whose designs were stolen by German immigrant Erwin Halstrup, and passed off as his own (the "Halstrup–Baumann artificial kidney").
[38] By the 1950s, Willem Kolff's invention of the dialyzer was used for acute renal failure, but it was not seen as a viable treatment for patients with stage 5 chronic kidney disease (CKD).
Swedish professor Nils Alwall[39] encased a modified version of this kidney inside a stainless steel canister, to which a negative pressure could be applied, in this way effecting the first truly practical application of hemodialysis, which was done in 1946 at the University of Lund.
Subsequently, he used such shunts, made of glass, as well as his canister-enclosed dialyzer, to treat 1500 patients in renal failure between 1946 and 1960, as reported to the First International Congress of Nephrology held in Evian in September 1960.
Subsequently, he collaborated with Swedish businessman Holger Crafoord to found one of the key companies that would manufacture dialysis equipment in the past 50 years, Gambro.
[40] Belding H. Scribner, working with the biomechanical engineer Wayne Quinton, modified the glass shunts used by Alwall by making them from Teflon.
For a detailed history of successful and unsuccessful attempts at dialysis, including pioneers such as Abel and Roundtree, Haas, and Necheles, see this review by Kjellstrand.