Passive smoking
It occurs when tobacco smoke diffuses into the surrounding atmosphere as an aerosol pollutant, which leads to its inhalation by nearby bystanders within the same environment.
[citation needed] In 1992, a review estimated that secondhand smoke exposure was responsible for 35,000 to 40,000 deaths per year in the United States in the early 1980s.
A 1997 meta-analysis found that secondhand smoke exposure increased the risk of heart disease by a quarter,[84] and two 1999 meta-analyses reached similar conclusions.
[95] Another meta-analysis confirmed the finding of an increased risk of lung cancer among women with spousal exposure to secondhand smoke the following year.
[101][102] The National Asthma Council of Australia cites studies showing that secondhand smoke is probably the most important indoor pollutant, especially around young children:[103] In France, exposure to secondhand smoke has been estimated to cause between 3,000[104] and 5,000 premature deaths per year, with the larger figure cited by Prime Minister Dominique de Villepin during his announcement of a nationwide smoke-free law: "That makes more than 13 deaths a day.
The US Surgeon General, in his 2006 report, estimated that living or working in a place where smoking is permitted increases the non-smokers' risk of developing heart disease by 25–30% and lung cancer by 20–30%.
[110] Similarly, children who are exposed to environmental tobacco smoke are shown to experience a range of adverse effects[111][112][113] and a higher risk of becoming smokers later in life.
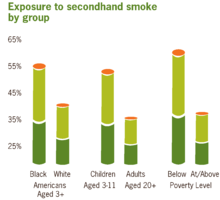
[115] The US Centers for Disease Control and Prevention monitors the extent of and trends in exposure to environmental tobacco smoke by measuring serum cotinine in national health surveys.
Carbon monoxide monitored through breath, nicotine, cotinine, thiocyanates, and proteins are the most specific biological markers of tobacco smoke exposure.
A 2004 study by the International Agency for Research on Cancer of the World Health Organization concluded that non-smokers are exposed to the same carcinogens as active smokers.
In an experiment conducted by the Italian National Cancer Institute, three cigarettes were left smoldering, one after the other, in a 60 m3 garage with a limited air exchange.
[128] Secondhand smoke exposure also affects platelet function, vascular endothelium, and myocardial exercise tolerance at levels commonly found in the workplace.
[153][154] A 2003 study by James Enstrom and Geoffrey Kabat, published in the British Medical Journal, argued that the harms of passive smoking had been overstated.
"[170] Steven Milloy, the "junk science" commentator for Fox News and a former Philip Morris consultant,[171][172] claimed that "of the 19 studies" on passive smoking "only 8— slightly more than 42%— reported statistically significant increases in heart disease incidence.
Milloy, who has a master's degree from the Johns Hopkins School of Hygiene and Public Health, argued that studies yielding relative risks of less than 2 were meaningless junk science.
[175] However, this effort was largely abandoned when it became clear that no independent epidemiological organization would agree to the standards proposed by Philip Morris et al.[176] In 1995, Levois and Layard, both tobacco industry consultants, published two analyses in the journal Regulatory Toxicology and Pharmacology regarding the association between spousal exposure to secondhand smoke and heart disease.
"[180] An accompanying editorial summarized: When all the evidence, including the important new data reported in this issue of the Journal, is assessed, the inescapable scientific conclusion is that ETS is a low-level lung carcinogen.
[188] A WHO inquiry, conducted after the release of the tobacco-industry documents, found that this controversy was generated by the tobacco industry as part of its larger campaign to cut the WHO's budget, distort the results of scientific studies on passive smoking, and discredit the WHO as an institution.
This campaign was carried out using a network of ostensibly independent front organizations and international and scientific experts with hidden financial ties to the industry.
[195] In a specific example which came to light with the release of tobacco-industry documents, Philip Morris executives successfully encouraged an author to revise his industry-funded review article to downplay the role of secondhand smoke in sudden infant death syndrome.
[198] Philip Morris reported that it was putting "...vast amounts of funding into these projects... in attempting to coordinate and pay so many scientists on an international basis to keep the ETS controversy alive.
Some (such as British American Tobacco and Philip Morris) acknowledge the medical consensus that secondhand smoke carries health risks, while others continue to assert that the evidence is inconclusive.
[206] Almost 7 years later, on August 17, 2006, U.S. District Court Judge Gladys Kessler found that the Government had proven its case and that the tobacco company defendants had violated the Racketeer Influenced Corrupt Organizations Act (RICO).
Admissions in neighbouring towns without smoke-free laws showed no change, and the decline in heart attacks in Pueblo was attributed to the resulting reduction in secondhand smoke exposure.
[109] A 2016 review also found that bans and policy changes in specific locations such as hospitals or universities can lead to reduced smoking rates.
[216] In 2001, a systematic review for the Guide to Community Preventive Services acknowledged strong evidence of the effectiveness of smoke-free policies and restrictions in reducing expose to secondhand smoke.
The examined studies provided sufficient evidence that smoke-free policies reduce tobacco use among workers when implemented in worksites or by communities.
[219] Recent surveys taken by the Society for Research on Nicotine and Tobacco demonstrate supportive attitudes of the public towards smoke-free policies in outdoor areas.
For example, critics of smoke-free laws cite studies suggesting ventilation as a means of reducing tobacco smoke pollutants and improving air quality.
[203][224] The implementation guidelines for the WHO Framework Convention on Tobacco Control states that engineering approaches, such as ventilation, are ineffective and do not protect against secondhand smoke exposure.