Statin
[1] Low-density lipoprotein (LDL) carriers of cholesterol play a key role in the development of atherosclerosis and coronary heart disease via the mechanisms described by the lipid hypothesis.
[2][3][4] Side effects of statins include muscle pain, increased risk of diabetes, and abnormal blood levels of certain liver enzymes.
The association between effect size and LDL cholesterol reduction was unclear, and there was significant clinical and statistical heterogeneity between trials.
[17] Clinical practice guidelines generally recommend that people at low risk start with lifestyle modification through a cholesterol-lowering diet and physical exercise; for those unable to meet their lipid-lowering goals through such methods, statins can be helpful.
[23] They recommended selective use of low-to-moderate doses statins in the same adults who have a calculated 10-year cardiovascular disease event risk of 7.5–10% or greater.
[23] In people over the age of 70, statins decrease the risk of cardiovascular disease but only in those with a history of heavy cholesterol blockage in their arteries.
[28] Two other meta-analyses published that year, one of which used data obtained exclusively from women, found no mortality benefit in primary prevention.
[29][30] The National Institute for Health and Clinical Excellence (NICE) recommends statin treatment for adults with an estimated 10 year risk of developing cardiovascular disease that is greater than 10%.
In this latter group, statin assignment was not automatic, but was recommended to occur only after a clinician-patient risk discussion with shared decision making where other risk factors and lifestyle are addressed, the potential for benefit from a statin is weighed against the potential for adverse effects or drug interactions and informed patient preference is elicited.
Defining illnesses include a prior heart attack, stroke, stable or unstable angina, aortic aneurysm, or other arterial ischemic disease, in the presence of atherosclerosis.
However, two large studies (HPS and PROSPER) that included people with vascular diseases reported that simvastatin and pravastatin did not impact cognition.
[56] In people with homozygous deficiencies, statins may still prove helpful, albeit at high doses and in combination with other cholesterol-reducing medications.
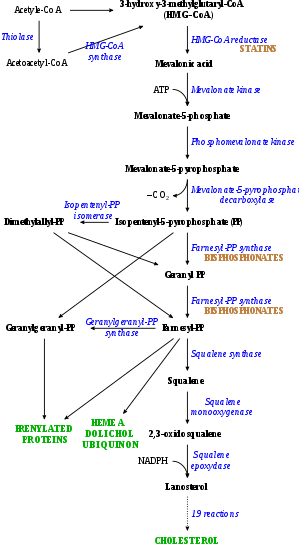
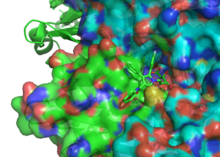
[35] This could be due to the statins inhibiting the enzyme (HMG-CoA reductase), which is necessary to make cholesterol, but also for other processes, such as CoQ10 production, which is important for muscle function and sugar regulation.
[77][78][79][80][81] A 2010 meta-review of medical trials involving over 65,000 people concluded that Statins decreased the risk of dementia, Alzheimer's disease, and even improved cognitive impairment in some cases.
[85] The U.S. Food and Drug Administration (FDA) package insert on statins includes a warning about the potential for non-serious and reversible cognitive side effects with the medication (memory loss, confusion).
A 2021 double-blind multiple crossover randomized controlled trial (RCT) in statin-intolerant patients found that adverse effects, including muscle pain, were similar between atorvastatin and placebo.
[95][96] Coenzyme Q10 (ubiquinone) levels are decreased in statin use;[97] CoQ10 supplements are sometimes used to treat statin-associated myopathy, though evidence of their efficacy is lacking as of 2017[update].
[99] Records exist of over 250,000 people treated from 1998 to 2001 with the statin drugs atorvastatin, cerivastatin, fluvastatin, lovastatin, pravastatin, and simvastatin.
However, the risk was over 10-fold greater if cerivastatin was used, or if the standard statins (atorvastatin, fluvastatin, lovastatin, pravastatin, or simvastatin) were combined with a fibrate (fenofibrate or gemfibrozil) treatment.
[100] Monitoring liver enzymes and creatine kinase is especially prudent in those on high-dose statins or in those on statin/fibrate combinations, and mandatory in the case of muscle cramps or of deterioration in kidney function.
[129] Furanocoumarins in grapefruit juice (i.e. bergamottin and dihydroxybergamottin) inhibit the cytochrome P450 enzyme CYP3A4, which is involved in the metabolism of most statins (however, it is a major inhibitor of only lovastatin, simvastatin, and to a lesser degree, atorvastatin) and some other medications[130] (flavonoids (i.e. naringin) were thought to be responsible).
[156] Researchers hypothesize that statins prevent cardiovascular disease via four proposed mechanisms (all subjects of a large body of biomedical research):[155] In 2008, the JUPITER trial showed statins provided benefit in those who had no history of high cholesterol or heart disease, but only in those with elevated high-sensitivity C-reactive protein (hsCRP) levels, an indicator for inflammation.
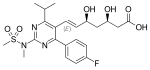
Cerivastatin is the most potent (withdrawn from the market in August 2001 due to risk of serious rhabdomyolysis), followed by (in order of decreasing potency) rosuvastatin, atorvastatin, simvastatin, lovastatin, pravastatin, and fluvastatin.
Treatment consisted mainly of dietary measures, such as a low-fat diet, and poorly tolerated medicines, such as clofibrate, cholestyramine, and nicotinic acid.
[citation needed] A British group isolated the same compound from Penicillium brevicompactum, named it compactin, and published their report in 1976.
P. Roy Vagelos, chief scientist and later CEO of Merck & Co, was interested, and made several trips to Japan starting in 1975.
"[194] As of 2016[update] misleading claims exaggerating the adverse effects of statins had received widespread media coverage, with a consequent negative impact to public health.
Cardiologist Steven Nissen at Cleveland Clinic commented "We are losing the battle for the hearts and minds of our patients to Web sites..."[196] promoting unproven medical therapies.
Harriet Hall sees a spectrum of "statin denialism" ranging from pseudoscientific claims to the understatement of benefits and overstatement of side effects, all of which is contrary to the scientific evidence.
[224] A modelling study in the UK funded by the NIHR found that people aged 70 and older who take statins live longer in good health than those who do not, regardless of whether they have cardiovascular disease.