Subdural hematoma
In contrast, epidural hematomas are usually caused by rips in arteries, resulting in a build-up of blood between the dura mater and the skull.
[3] It is often claimed that subdural hematoma is a common finding in shaken baby syndrome, although there is no science to support this.
[12] Other risk factors include taking blood thinners (anticoagulants), long-term excessive alcohol consumption, dementia, and cerebrospinal fluid leaks.
Matrix metalloproteinases remove surrounding collagen, providing space for new blood vessels to grow.
[16] Craniotomy for unruptured intracranial aneurysm is another risk factor for the development of chronic subdural hematoma.
The incision in the arachnoid membrane during the operation causes cerebrospinal fluid to leak into the subdural space, leading to inflammation.
[17] It is important that a person receive medical assessment, including a complete neurological examination, after any head trauma.
[3] Unlike epidural hematomas, which cannot expand past the sutures of the skull, subdural hematomas can expand along the inside of the skull, creating a concave shape that follows the curve of the brain, stopping only at dural reflections like the tentorium cerebelli and falx cerebri.
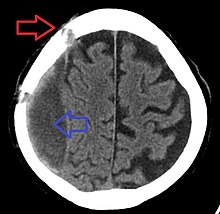
[citation needed] On a CT scan, subdural hematomas are classically crescent-shaped, with a concave surface away from the skull.
In such cases, subtle signs of bleeding—such as effacement of sulci or medial displacement of the junction between gray matter and white matter—may be apparent.
[citation needed] Fresh subdural bleeding is hyperdense, but becomes more hypodense over time due to dissolution of cellular elements.
Acute subdural hematomas due to trauma are the most lethal of all head injuries and have a high mortality rate if they are not rapidly treated with surgical decompression.
[24] Chronic subdural bleeds develop over a period of days to weeks, often after minor head trauma, though a cause is not identifiable in 50% of patients.
In one study, only 22% of patients with chronic subdural bleeds had outcomes worse than "good" or "complete recovery".
Some small subdural hematomas can be managed by careful monitoring as the blood clot is eventually resorbed naturally.
A surgeon opens the skull and then the dura mater; removes the clot with suction or irrigation; and identifies and controls sites of bleeding.
Postoperative complications can include increased intracranial pressure, brain edema, new or recurrent bleeding, infection, and seizures.
[32] HMG-CoA reductase inhibitor such as Atorvastatin can reduce the haematoma volume and improving neurological function in eight weeks.