Symptoms of COVID-19
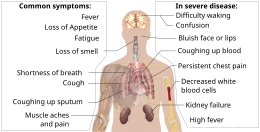
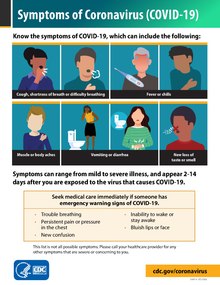
[1][2] Common symptoms include coughing, fever, loss of smell (anosmia) and taste (ageusia), with less common ones including headaches, nasal congestion and runny nose, muscle pain, sore throat, diarrhea, eye irritation,[3] and toes swelling or turning purple,[4] and in moderate to severe cases, breathing difficulties.
Many COVID-19 patients with co-morbidities have hypoxia and have been in intensive care for varying lengths of time, confounding interpretation of the data.
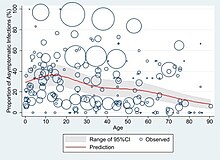
[10][needs update] At least a third of the people who are infected with the virus do not develop noticeable symptoms at any point in time.
However, some people continue to experience a range of effects, such as fatigue, for prolonged periods after an initial COVID-19 infection.
[20] This is the result of a condition called long COVID, which can be described as a range of persistent symptoms that continue for months or years.
[20] Reducing the risk of long COVID includes staying up to date on the most recent COVID-19 vaccine, practicing good hygiene, maintaining clean indoor air, and physical distancing from people infected with a respiratory virus.
[1] Further development of the disease can lead to complications including pneumonia, acute respiratory distress syndrome, sepsis, septic shock, and kidney failure.
[23] In August 2020, scientists at the University of Southern California reported the "likely" order of initial symptoms of the COVID-19 disease as a fever followed by a cough and muscle pain, and that nausea and vomiting usually appear before diarrhea.
People infected with the Delta variant may mistake the symptoms for a bad cold and not realize they need to isolate.
Common symptoms reported as of June 2021 have been headaches, sore throat, runny nose, and fever.
[28][medical citation needed][29] British epidemiologist Tim Spector said in mid-December 2021 that the majority of symptoms of the Omicron variant were the same as a common cold, including headaches, sore throat, runny nose, fatigue and sneezing, so that people with cold symptoms should take a test.
Persistent anosmia or hyposmia or ageusia or dysgeusia has been documented in 20% of cases for longer than 30 days.
Similarly, the level of inflammation-related markers such as C-reactive protein (CRP), D-dimer, IL-6, procalcitonin was significantly increased, indicating an inflammatory process in the body.
Electrocardiogram findings were variable and ranged from sinus tachycardia, ST-segment elevation, T-wave inversion and ST-depression.
[49][50] Endomyocardial biopsy [EMB] remains the gold standard invasive technique in diagnosing myocarditis; however, due to the increased risk of infection, it is not done in COVID-19 patients.
[citation needed] The binding of the SARS-CoV-2 virus through ACE2 receptors present in heart tissue may be responsible for direct viral injury leading to myocarditis.
[5] A disturbance in smell or taste is more commonly found in younger people, and perhaps because of this, it is correlated with a lower risk of medical complications.
Some reported symptoms include delirium, stroke, brain hemorrhage, memory loss, psychosis, peripheral nerve damage, anxiety, and post-traumatic stress disorder.
[63] As of September 2020, it was unclear whether these symptoms were due to direct infection of brain cells, or of overstimulation of the immune system.
[2] Patients are at increased risk of a range of different blood clots, some potentially fatal, for months following COVID infection.
[36][37][38][39][excessive citations] There are three stages, according to the way COVID-19 infection can be tackled by pharmacological agents, in which the disease can be classified.
[71] Stage I is the early infection phase during which the domination of upper respiratory tract symptoms is present.
[78] In people requiring hospital admission, up to 98% of CT scans performed show lung abnormalities after 28 days of illness even if they had clinically improved.
[79] People with advanced age, severe disease, prolonged ICU stays, or who smoke are more likely to have long-lasting effects, including pulmonary fibrosis.
[80] Overall, approximately one-third of those investigated after four weeks will have findings of pulmonary fibrosis or reduced lung function as measured by DLCO, even in asymptomatic people, but with the suggestion of continuing improvement with the passing of more time.
[78] After severe disease, lung function can take anywhere from three months to a year or more to return to previous levels.
[83] Long COVID can be present in anyone who has contracted COVID-19 at some point; typically, it is more commonly found in those who had severe illness due to the virus.
[83][84] Long COVID can attack a multitude of organs such as the lungs, heart, blood vessels, kidneys, gut, and brain.
[85] Some common symptoms that occur as a result are fatigue, cough, shortness of breath, chest pains, brain fog, gastrointestinal issues, insomnia, anxiety/depression, and delirium.
People are found to be dealing with brain fog and impaired memory, and diminished learning ability which has a large impact on their everyday lives.