Smoking cessation
In recent years, especially in Canada and the United Kingdom, many smokers have switched to using electronic cigarettes to quit smoking tobacco.
[16][17][18] However, a 2022 study found that 20% of smokers who tried to use e-cigarettes to quit smoking succeeded but 66% of them ended as dual users of cigarettes and vape products one year out.
A 2009 systematic review by researchers at the University of Birmingham found that gradual nicotine replacement therapy could be effective in smoking cessation.
When reducing the number of smoked cigarettes, it found some evidence that additional varenicline or fast-acting nicotine replacement therapy can positively affect quitting for six months or longer.
[33] The American Cancer Society notes that "Studies in medical journals have reported that about 25% of smokers who use medicines can stay smoke-free for over 6 months.
"[34] Single medications include: The 2008 US Guideline specifies that three combinations of medications are effective:[46]: 118–120 A meta-analysis from 2018, conducted on 61 RCTs, showed that during their first year of trying to quit, approximately 80% of the participants in the studies who got drug assistance (bupropion, NRT, or varenicline) returned to smoking, while 20% continued to not smoke for the entire year (i.e.: remained sustained abstinent).
In Malaysia, their study looked at how pharmacist intervention in patients' overall healthcare showed improvements in screening early stages of disease.
In pharmacist-led smoking cessation services in Ethiopia, the study found statistically and clinically significant benefits favouring pharmacist intervention.
[99] In Nepal, smokers are not selfish, a health campaign of two weeks is started on the occasion of Valentine day and Vasant panchami to motiviate individuals to quit smoking as a sacrifice for their loved ones and making it a meaningful decision of life.
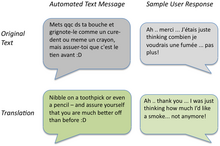
[46]: 89–91 Nevertheless, self-help modalities for smoking cessation include: Various methods allow a smoker to see the impact of their tobacco use and the immediate effects of quitting.
[119] A 2010 systematic review determined that worksite incentives and competitions needed to be combined with additional interventions to produce significant increases in smoking cessation rates.
It is important to note that most of the alternative approaches below have minimal evidence to support their use, and their efficacy and safety should be discussed with a healthcare professional before starting.
Methods used with children and adolescents include: Cochrane reviews, mainly of studies combining motivational enhancement and psychological support, concluded that "complex approaches" for smoking cessation among young people show promise.
The 2008 US Guideline determined that "person-to-person psychosocial interventions" (typically including "intensive counseling") increased abstinence rates in pregnant women who smoke to 13.3%, compared with 7.6% in usual care.
In addition, these babies have weaker immune systems, making them more susceptible to many diseases such as middle ear inflammations and asthmatic bronchitis, as well as metabolic conditions such as diabetes and hypertension, all of which can bring significant morbidity.
[160] Additionally, a study published by American Academy of Pediatrics shows that smoking during pregnancy increases the chance of sudden unexpected infant death ((SUID) or (SIDS)).
A systematic review showed that psychosocial interventions help women quit smoking in late pregnancy and can reduce the incidence of low birth weight infants.
[164][165] However, life style modification are the preferred method for pregnant women, and they should discuss smoking cessation techniques with a healthcare professional.
[46]: 149–150 A 2012 Cochrane review found that interventions beginning during a hospital stay and continuing for one month or more after discharge were effective in producing abstinence.
[172] Exposure to cigarette smoke early on in life, during pregnancy, infancy, or adolescence, may negatively impact a child's neurodevelopment and increase the risk of developing anxiety disorders in the future.
The emphasis of immediate financial benefits to those who concern themselves with the short-term over the long-term, partnering with shelters to reduce the social acceptability of smoking in this population, and increased taxes on cigarettes and alternative tobacco products to further make the addiction more difficult to fund.
[177][178] Providing behavioural interventions (such as counseling and advice) and pharmacotherapy including nicotine replacement therapy (such as the use of patches or gum, varenicline, and/or bupropion) increase tobacco abstinence that is sustainable and also reduces the risk of returning to other substance use.
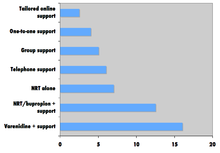
[182] Robert West and Saul Shiffman, authorities in this field recognized by government health departments in a number of countries,[168]: 73, 76, 80 have concluded that, used together, "behavioral support" and "medication" can quadruple the chances that a quit attempt will be successful.
Studies suggest this can cause the phenomenon of increased nicotine dependence and lower smoking cessation rate in darker-pigmented individuals.
[186] Nevertheless, a Cochrane review determined that interventions to increase social support for a smoker's cessation attempt did not improve long-term quit rates.
Therefore, if an acquaintance offers a cigarette as a polite gesture, the person who has stopped smoking will be likelier to break his commitment than if a friend had suggested it.
[210] A 2013 study by The British Journal of Psychiatry has found that smokers who successfully quit feel less anxious afterward, with the effect being greater among those who had mood and anxiety disorders than those who smoked for pleasure.
[212] Randomized U.S. and Canadian trials showed that a ten-week smoking cessation program decreased mortality from all causes over 14 years later.
[214] A recent article on mortality in a cohort of 8,645 smokers who were followed up after 43 years determined that "current smoking and lifetime persistent smoking were associated with an increased risk of all-cause, CVD [cardiovascular disease], COPD [chronic obstructive pulmonary disease], and any cancer, and lung cancer mortality.
[218] Cost-effectiveness analyses of smoking cessation activities have shown that they increase quality-adjusted life years (QALYs) at costs comparable with other types of interventions to treat and prevent disease.