Traumatic cardiac arrest
Traumatic cardiac arrest (TCA) is a condition in which the heart has ceased to beat due to blunt or penetrating trauma, such as a stab wound to the thoracic area.
[4] In both blunt and penetrating trauma, massive internal or external bleeding may decrease the volume of blood is available to be pumped by the heart to the body.
In the setting of trauma, cardiac tamponade results from an acute pericardial effusion, the accumulation of blood within the sac that surrounds the heart.
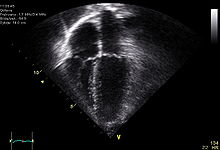
Clinicians will also order diagnostic testing that may include chest x-ray, bedside ultrasound and echocardiogram, and blood gas levels.
Other work-up involved in diagnosis of a trauma patient may include e-FAST, RUSH exam, CBC, pelvic X-ray, and CT of the head, neck, chest, abdomen, and pelvis.
Additionally, as many of the interventions targeted at specific causes of arrest are centered around procedures performed around the patient's chest, head, and neck, compressions may interfere with definitive management.
[3] Evolving algorithms are directed at quickly identifying incidences of cardiac arrest with a traumatic source and rapidly intervening to address reversible causes.
[6] There is wide variability in the estimated survival rate based on factors that include initiation of pre-hospital care and nature of injury.
A 2012 review suggests that while survival rates of traumatic cardiac arrest are higher in children, so is the incidence of neurological complication.