Vitamin B12 deficiency
[1] In moderate deficiency, feeling tired, headaches, soreness of the tongue, mouth ulcers, breathlessness, feeling faint, rapid heartbeat, low blood pressure, pallor, hair loss, decreased ability to think and severe joint pain and the beginning of neurological symptoms, including abnormal sensations such as pins and needles, numbness and tinnitus may occur.
[1] Severe deficiency may include symptoms of reduced heart function as well as more severe neurological symptoms, including changes in reflexes, poor muscle function, memory problems, blurred vision, irritability, ataxia, decreased smell and taste, decreased level of consciousness, depression, anxiety, guilt and psychosis.
[8] Other conditions giving rise to malabsorption include surgical removal of the stomach, chronic inflammation of the pancreas, intestinal parasites, certain medications such as long-term use of proton pump inhibitors, H2-receptor blockers, and metformin, and some genetic disorders.
[15][16][17] A mild deficiency may not cause any discernible symptoms, but at levels moderately lower than normal, a range of symptoms such as feeling tired, weak, lightheadedness, headaches, dizziness, rapid breathing, rapid heartbeat, cold hands and feet, low-grade fevers, tremor, cold intolerance, easy bruising and bleeding, pale skin, low blood pressure, sore tongue, upset stomach, loss of appetite, weight loss, constipation, diarrhea, severe joint pain, feeling abnormal sensations including numbness or tingling (pins and needles) to the fingers and toes, and tinnitus, may be experienced.
[18][19][20][21] A wide range of associated symptoms may include angular cheilitis, mouth ulcers, bleeding gums, hair loss and thinning, premature greying, a look of exhaustion and dark circles around the eyes, as well as brittle nails.
[30] Pernicious anemia is a disease caused by an autoimmune response that produces antibodies that attack the parietal cells in the stomach lining, preventing them from creating intrinsic factor needed for the absorption of vitamin B12.
[39] Furthermore, an animal study in ewes demonstrated that a B12, folate and methionine restricted diet around conception, resulted in offspring with higher adiposity, blood pressure and insulin resistance which could be accounted for by altered DNA methylation patterns.
[45] Vitamin B12 deficiency has the potential to influence methylation patterns in DNA, besides other epigenetic modulators such as micro (RNAs), leading to the altered expression of genes.
In addition it has been associated with adverse foetal and neonatal outcomes including neural tube defects (NTDs)[50][51][52][53] and delayed myelination or demyelination.
[37][54] The mother's B12 status can be important in determining the later health of the child, as shown in the Pune maternal Nutrition Study, conducted in India.
[41] Increased longitudinal cohort studies or randomised controlled trials are required to understand the mechanisms between vitamin B12 and metabolic outcomes, and to potentially offer interventions to improve maternal and offspring health.
[56][57][58] A long-term study where vitamin B12 was supplemented across a period of 10 years, led to lower levels of weight gain in overweight or obese individuals (p < 0.05).
If this reaction cannot occur, methylmalonyl-CoA levels elevate, inhibiting the rate-limiting enzyme of fatty acid oxidation (CPT1 – carnitine palmitoyl transferase), leading to lipogenesis and insulin resistance.
[72][73][74][75] Finally, a recent literature review conducted over 19 studies, found no evidence of an inverse association between BMI and circulating vitamin B12.
[82] Furthermore, obese individuals with type 2 diabetes are likely to develop gastroesophageal reflux disease,[83] and take proton pump inhibitors, which further increased the risk of vitamin B12 deficiency.
[71] A literature review conducted in 2011 over seven studies, found that there was limited evidence to show that low vitamin B12 status increased the risk of cardiovascular disease and diabetes.
In a dose-response meta-analysis of five prospective cohort studies, it was reported that the risk of coronary heart disease (CHD) did not change substantially with increasing dietary vitamin B12 intake.
However, the overall contribution of vitamin B12 deficiency to the global incidence of anemia may not be significant, except in elderly individuals, vegetarians, cases of malabsorption and some genetic disorders.
Megaloblastic anemia caused by vitamin B12 deficiency is characterized by red blood cells that are larger than normal and are unable to deliver oxygen to the body's organs.
[7][8] The clinical case indicates an altered synthesis of DNA, in which vitamin B12 is essential for the production and maturation of red blood cells in the bone marrow.
[91][92] Several risk factors have been linked to macular degeneration, including family history, genetics, hypercholesterolemia, hypertension, sunlight exposure and lifestyle (smoking and diet).
[96] However, another study failed to find an association between age-related macular degeneration and vitamin B12 status in a sample of 3,828 individuals representative of the non-institutionalized US population.
[104][105][106] In advanced stages of vitamin B12 deficiency, cases of psychosis, paranoia and severe depression have been observed, which may lead to permanent disability if left untreated.
[2] Inadequate dietary intake of animal products such as eggs, meat, milk, fish, fowl (and some types of edible algae) can result in a deficiency state.
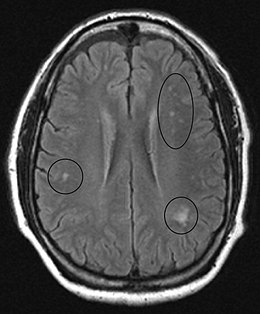
In the brain itself, changes are less severe: They occur as small sources of nervous fibers decay and accumulation of astrocytes, usually subcortically located, and also round hemorrhages with a torus of glial cells.
[147] If nervous system damage is present and blood testing is inconclusive, a lumbar puncture to measure cerebrospinal fluid B-12 levels may be done.
[157] The data from the National Health and Nutrition Examination Survey (NHANES) reported the prevalence of serum vitamin B12 concentrations in the United States population between 1999 and 2002.
These surveys have reported a high prevalence of vitamin B12 deficiency (< 150 pmol/L), among 36% of breastfed and 9% of non-breastfed children (n = 2482) in New Delhi[169] and 47% of adults (n = 204)[170] in Pune, Maharashtra, India.
William Castle demonstrated that gastric juice contained an "intrinsic factor" which when combined with meat ingestion resulted in absorption of the vitamin in this condition.
[177][176] The "coast disease" of sheep in the coastal sand dunes of South Australia in the 1930s was found to originate in nutritional deficiencies of the trace elements, cobalt and copper.