Paracetamol poisoning
This is typically followed by absence of symptoms for a couple of days, after which yellowish skin, blood clotting problems, and confusion occurs as a result of liver failure.
Additional complications may include kidney failure, pancreatitis, low blood sugar, and lactic acidosis.
The first phase begins within hours of overdose, and consists of nausea, vomiting, a pale appearance, and sweating.
Rarely, after massive overdoses, patients may develop symptoms of metabolic acidosis and coma early in the course of poisoning.
Hallmark pathology on liver biopsy includes regions of coagulative necrosis in zone 3 of the liver acinus, around the central venules, as these hepatocytes have higher concentrations of cytochrome P450 enzymes compared to zone 1 hepatocytes surrounding the portal venule of the acinus.
In adults, single doses above 10 grams or 200 mg/kg of bodyweight, whichever is lower, have a reasonable likelihood of causing toxicity.
[22] Studies have shown significant hepatotoxicity is uncommon in patients who have taken greater than normal doses over 3 to 4 days.
[32][33] Concomitant use of other drugs that induce CYP enzymes, such as antiepileptics including carbamazepine, phenytoin, and barbiturates, have also been reported as risk factors.
[14] Following a therapeutic dose, it is mostly converted to nontoxic metabolites via Phase II metabolism by conjugation with sulfate and glucuronide, with a small portion being oxidized via the cytochrome P450 enzyme system.
[35] Cytochromes P450 2E1 and 3A4 convert approximately 5% of paracetamol to a highly reactive intermediary metabolite, N-acetyl-p-benzoquinone imine (NAPQI).
Use of a timed serum paracetamol level plotted on the nomogram appears to be the best marker indicating the potential for liver injury.
[44] Paracetamol may be quantified in blood, plasma, or urine as a diagnostic tool in clinical poisoning situations or to aid in the medicolegal investigation of suspicious deaths.
[52] In addition, alternative pain relief medications such as aspirin are more toxic in overdose, whereas non-steroidal anti-inflammatory drugs are associated with more adverse effects following normal use.
[53] One strategy for reducing harm done by acetaminophen overdoses is selling paracetamol pre-combined in tablets either with an emetic[52] or an antidote.
These results taken together with the good hydrolysis and bioavailability data show that this ester is a potential candidate as a prodrug of paracetamol.
Paracetamol absorption from the gastrointestinal tract is complete within two hours under normal circumstances, so decontamination is most helpful if performed within this timeframe.
[63][62] Administering activated charcoal later than 2 hours can be considered in patients that may have delayed gastric emptying due to co-ingested drugs or following ingestion of sustained- or delayed-release paracetamol preparations.
[42] There was reluctance to give activated charcoal in paracetamol overdose, because of the concern that it may also absorb the oral antidote acetylcysteine.
Children with accidental exposures do not require gastrointestinal decontamination with either gastric lavage, activated charcoal, or syrup of ipecac.
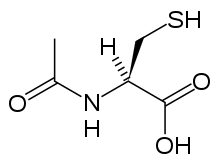
[20] Acetylcysteine, also called N-acetylcysteine or NAC, works to reduce paracetamol toxicity by replenishing body stores of the antioxidant glutathione.
[61] If the person presents less than eight hours after paracetamol overdose, then acetylcysteine significantly reduces the risk of serious hepatotoxicity and guarantees survival.
[71] If the person presents more than eight hours after the paracetamol overdose, then activated charcoal is not useful, and acetylcysteine is started immediately.
In earlier presentations, charcoal can be given when the patient arrives and acetylcysteine is initiated while waiting for the paracetamol level results to return from the laboratory.
[20] In United States practice, intravenous (IV) and oral administration are considered to be equally effective and safe if given within 8 hours of ingestion.
[75][76] Oral acetylcysteine may be poorly tolerated due to its unpleasant taste, odor, and its tendency to cause nausea and vomiting.
[78] The most common adverse effect to acetylcysteine treatment is an anaphylactoid reaction, usually manifested by rash, wheeze, or mild hypotension.
[79] Rarely, severe life-threatening reactions may occur in predisposed individuals, such as patients with asthma or atopic dermatitis, and may be characterized by respiratory distress, facial swelling, and even death.
[79][81][82] If an anaphylactoid reaction occurs the acetylcysteine is temporarily halted or slowed and antihistamines and other supportive care is administered.
The most commonly used criteria for liver transplant were developed by physicians at King's College Hospital in London.
It is estimated that 150 to 200 deaths and 15 to 20 liver transplants occur as a result of poisoning each year in England and Wales.