Alcoholic hepatitis
[4] It may also present with Hepatic encephalopathy (brain dysfunction due to liver failure) causing symptoms such as confusion, decreased levels of consciousness, or asterixis,[5] (a characteristic flapping movement when the wrist is extended indicative of hepatic encephalopathy).
Severe cases are characterized by profound jaundice, obtundation (ranging from drowsiness to unconsciousness), and progressive critical illness; the mortality rate is 50% within 30 days of onset despite best care.
[6] Some alcoholics develop acute hepatitis as an inflammatory reaction to the cells affected by fatty change.
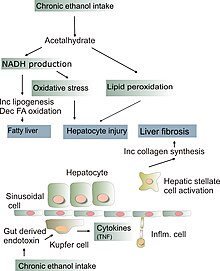
This inflammatory reaction to the fatty change is called alcoholic steatohepatitis and the inflammation probably predisposes to liver fibrosis by activating hepatic stellate cells to produce collagen.
[7] In the case of enterococcus faecalis, the bacterium can release an exotoxin which is directly damaging to liver cells.
[7] Chronic alcohol consumption may alter the gut microbiome and promote the production of these pathogenic bacteria.
[7] The chronic inflammation seen in alcoholic hepatitis leads to a distinctive fibrotic response, with fibrogenic cell type activation.
[7] This leads to defects in the liver's many functions including impairments in bilirubin transport, clotting factor synthesis, glucose metabolism and immune dysfunction.
Furthermore, decreased levels of IL-13, an antagonistic cytokine of IL-6 was found to be closely associated with short-term (90-day) mortality in severe alcoholic hepatitis patients.
[7] Certain genetic variations in the PNPLA3-encoding gene, which codes for an enzyme involved in triglyceride metabolism in adipose tissue are thought to influence disease severity.