Benzodiazepine
[1] By 1977, benzodiazepines were the most prescribed medications globally; the introduction of selective serotonin reuptake inhibitors (SSRIs), among other factors, decreased rates of prescription, but they remain frequently used worldwide.
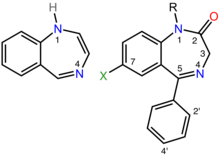
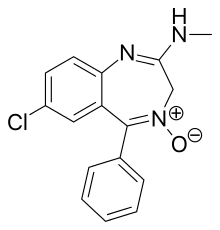
[2][3] Benzodiazepines are depressants that enhance the effect of the neurotransmitter gamma-aminobutyric acid (GABA) at the GABAA receptor, resulting in sedative, hypnotic (sleep-inducing), anxiolytic (anti-anxiety), anticonvulsant, and muscle relaxant properties.
[4] These properties make benzodiazepines useful in treating anxiety, panic disorder, insomnia, agitation, seizures, muscle spasms, alcohol withdrawal and as a premedication for medical or dental procedures.
[8] According to the Government of Victoria's (Australia) Department of Health, long-term use can cause "impaired thinking or memory loss, anxiety and depression, irritability, paranoia, aggression, etc.
[21][22][23] Benzodiazepines possess psycholeptic, sedative, hypnotic, anxiolytic, anticonvulsant, muscle relaxant, and amnesic actions,[4][5] which are useful in a variety of indications such as alcohol dependence, seizures, anxiety disorders, panic, agitation, and insomnia.
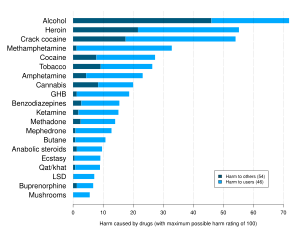
[29] Benzodiazepines can have serious adverse health outcomes, and these findings support clinical and regulatory efforts to reduce usage, especially in combination with non-benzodiazepine receptor agonists.
[34] American Psychiatric Association (APA) guidelines, published in January 2009,[34] note that, in general, benzodiazepines are well tolerated, and their use for the initial treatment for panic disorder is strongly supported by numerous controlled trials.
The choice of treatment between benzodiazepines, SSRIs, serotonin–norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants, and psychotherapy should be based on the patient's history, preference, and other individual characteristics.
Selective serotonin reuptake inhibitors are likely to be the best choice of pharmacotherapy for many patients with panic disorder, but benzodiazepines are also often used, and some studies suggest that these medications are still used with greater frequency than the SSRIs.
[40] Likewise, Canadian Psychiatric Association (CPA) recommends benzodiazepines alprazolam, bromazepam, lorazepam, and diazepam only as a second-line choice, if the treatment with two different antidepressants was unsuccessful.
Both are used in the detoxification of individuals who are motivated to stop drinking, and are prescribed for a short period of time to reduce the risks of developing tolerance and dependence to the benzodiazepine medication itself.
[62][63] Benzodiazepines are the preferred choice in the management of alcohol withdrawal syndrome, in particular, for the prevention and treatment of the dangerous complication of seizures and in subduing severe delirium.
This included hospitalization, patient transfer, or death, and visits involving a combination of benzodiazepines and non-benzodiapine receptor agonists had almost four-times increased odds of a serious health outcome.
[117] The short-term use of benzodiazepines adversely affects multiple areas of cognition, the most notable one being that it interferes with the formation and consolidation of memories of new material and may induce complete anterograde amnesia.
[115][118] This meta-analysis found that long-term use of benzodiazepines was associated with moderate to large adverse effects on all areas of cognition, with visuospatial memory being the most commonly detected impairment.
[123] While benzodiazepines may have short-term benefits for anxiety, sleep and agitation in some patients, long-term (i.e., greater than 2–4 weeks) use can result in a worsening of the very symptoms the medications are meant to treat.
[124][133] Tolerance and dependence are risks of chronic benzodiazepine use, and can result in doses within the therapeutic range ceasing to offer meaningful symptomatic relief after prolonged use.
[137] The less frequent effects are irritability, sweating, depersonalization, derealization, hypersensitivity to stimuli, depression, suicidal behavior, psychosis, seizures, and delirium tremens.
Abrupt withdrawal can be dangerous and lead to excitotoxicity, causing damage and even death to nerve cells as a result of excessive levels of the excitatory neurotransmitter glutamate.
[12] Symptoms may also occur during a gradual dosage reduction, but are typically less severe and may persist as part of a protracted withdrawal syndrome for months after cessation of benzodiazepines.
A goal of less than six months has been suggested,[12] but due to factors such as dosage and type of benzodiazepine, reasons for prescription, lifestyle, personality, environmental stresses, and amount of available support, a year or more may be needed to withdraw.
[171][172] The symptoms of a benzodiazepine overdose may include; drowsiness, slurred speech, nystagmus, hypotension, ataxia, coma, respiratory depression, and cardiorespiratory arrest.
It is contraindicated in people with a history of long-term use of benzodiazepines, those having ingested a substance that lowers the seizure threshold or may cause an arrhythmia, and in those with abnormal vital signs.
In contrast, drugs that induce cytochrome P450 enzymes, such as St John's wort, the antibiotic rifampicin, and the anticonvulsants carbamazepine and phenytoin, accelerate elimination of many benzodiazepines and decrease their action.
[207] The court case against the drug manufacturers never reached a verdict; legal aid had been withdrawn and there were allegations that the consultant psychiatrists, the expert witnesses, had a conflict of interest.
[209] Although antidepressants with anxiolytic properties have been introduced, and there is increasing awareness of the adverse effects of benzodiazepines, prescriptions for short-term anxiety relief have not significantly dropped.
[229] Dependence and tolerance, often coupled with dosage escalation, to benzodiazepines can develop rapidly among people who misuse drugs; withdrawal syndrome may appear after as little as three weeks of continuous use.
Long-term use has the potential to cause both physical and psychological dependence and severe withdrawal symptoms such as depression, anxiety (often to the point of panic attacks), and agoraphobia.
[16] Benzodiazepines and, in particular, temazepam are sometimes used intravenously, which, if done incorrectly or in an unsterile manner, can lead to medical complications including abscesses, cellulitis, thrombophlebitis, arterial puncture, deep vein thrombosis, and gangrene.
Non-medical temazepam use reached epidemic proportions in some parts of the world, in particular, in Europe and Australia, and is a major addictive substance in many Southeast Asian countries.