Anemia
[5] When anemia comes on slowly, the symptoms are often vague, such as tiredness, weakness, shortness of breath, headaches, and a reduced ability to exercise.
[1] When anemia is acute, symptoms may include confusion, feeling like one is going to pass out, loss of consciousness, and increased thirst.
A patient with anemia may report feeling tired, weak, decreased ability to concentrate, and sometimes shortness of breath on exertion.
[20][24] Symptoms can include feeling tired, weak, dizziness, headaches, intolerance to physical exertion, shortness of breath, difficulty concentrating, irregular or rapid heartbeat, cold hands and feet, cold intolerance, pale or yellow skin, poor appetite, easy bruising and bleeding, and muscle weakness.
[23] Anemia that develops quickly, often, has more severe symptoms, including, feeling faint, chest pain, sweating, increased thirst, and confusion.
Iron-deficiency anemia may give symptoms that can include spoon-shaped nails, restless legs syndrome, and pica (the medical condition indicates the desire for things that are not food, such as ice, dirt, etc.).
[30] Vitamin B12 deficiency anemia may result in decreased ability to think, memory loss, confusion, personality or mood changes, depression, difficulty walking, blurred vision, and irreversible nerve damage.
In severe anemia, there may be signs of a hyperdynamic circulation: tachycardia (a fast heart rate), bounding pulse, flow murmurs, and cardiac ventricular hypertrophy (enlargement).
Pica, the consumption of non-food items such as ice, paper, wax, grass, hair or dirt, may be a symptom of iron deficiency;[29] although it occurs often in those who have normal levels of hemoglobin.
The mechanisms involved are multifactorial and not limited to malabsorption but mainly related to chronic intestinal inflammation, which causes dysregulation of hepcidin that leads to decreased access of iron to the circulation.
[64] An operational definition is a decrease in whole-blood hemoglobin concentration of more than 2 standard deviations below the mean of an age- and sex-matched reference range.
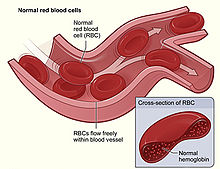
[65] It is difficult to directly measure RBC mass,[66] so the hematocrit (amount of RBCs) or the hemoglobin (Hb) in the blood are often used instead to indirectly estimate the value.
For example, during pregnancy a woman's RBC mass is normal but because of an increase in blood volume the hemoglobin and hematocrit are diluted and thus decreased.
Another example would be bleeding where the RBC mass would decrease but the concentrations of hemoglobin and hematocrit initially remains normal until fluids shift from other areas of the body to the intravascular space.
Examination of a stained blood smear using a microscope can also be helpful, and it is sometimes a necessity in regions of the world where automated analysis is less accessible.
In clinical workup, the MCV will be one of the first pieces of information available, so even among clinicians who consider the "kinetic" approach more useful philosophically, morphology will remain an important element of classification and diagnosis.
This classification depends on evaluation of several hematological parameters, particularly the blood reticulocyte (precursor of mature RBCs) count.
The Mentzer index (mean cell volume divided by the RBC count) predicts whether microcytic anemia may be due to iron deficiency or thalassemia, although it requires confirmation.
The nonmegaloblastic macrocytic anemias have different etiologies (i.e. unimpaired DNA globin synthesis,) which occur, for example, in alcoholism.
[83] Normocytic anemia occurs when the overall hemoglobin levels are decreased, but the red blood cell size (mean corpuscular volume) remains normal.
Evidence for multiple causes appears with an elevated RBC distribution width (RDW), indicating a wider-than-normal range of red cell sizes, also seen in common nutritional anemia.
[citation needed] Heinz bodies form in the cytoplasm of RBCs and appear as small dark dots under the microscope.
It may be drug-induced, for example in cats and dogs by acetaminophen (paracetamol),[84] or may be caused by eating various plants or other substances: Hyperanemia is a severe form of anemia, in which the hematocrit is below 10%.
[89] Iron-deficiency anemia may also be refractory as a manifestation of gastrointestinal problems which disrupt iron absorption or cause occult bleeding.
The diagnosis of iron deficiency mandates a search for potential sources of blood loss, such as gastrointestinal bleeding from ulcers or colon cancer.
[32] The objective for the administration of an erythropoiesis-stimulating agent (ESA) is to maintain hemoglobin at the lowest level that both minimizes transfusions and meets the individual person's needs.
[108][109] The 2020 Cochrane Anaesthesia Review Group review of erythropoietin (EPO) plus iron versus control treatment including placebo or iron for preoperative anaemic adults undergoing non-cardiac surgery [110] demonstrated that patients were much less likely to require red cell transfusion and in those transfused, the volumes were unchanged (mean difference -0.09, 95% CI -0.23 to 0.05).
[111][112] The use of HBO is indicated when oxygen delivery to tissue is not sufficient in patients who cannot be given blood transfusions for medical or religious reasons.
HBO may be used for medical reasons when threat of blood product incompatibility or concern for transmissible disease are factors.
[115] There is moderate level medical evidence that supports a combination of iron supplementation and erythropoietin treatment to help reduce the requirement for red blood cell transfusions after surgery in those who have preoperative anemia.