Combined oral contraceptive pill
[28] In this period, the pituitary gland located near the brain secretes follicle-stimulating hormone (FSH) into the bloodstream to signal the development of follicle in ovary in the female reproductive system.
[28] Specifically in ovulation, transient positive feedback by Oestrogen on FSH and Luteinising Hormone (LH) secretion from pituitary is permitted so that the release of mature ovum from follicle is triggered.
[30][31][32] Estrogen was originally included in oral contraceptives for better cycle control (to stabilize the endometrium and thereby reduce the incidence of breakthrough bleeding), but was also found to inhibit follicular development and help prevent ovulation.
[30][31][32] Another primary mechanism of action of all progestogen-containing contraceptives is inhibition of sperm penetration through the cervix into the upper genital tract (uterus and fallopian tubes) by decreasing the water content and increasing the viscosity of the cervical mucus.
Factors that may contribute to a decrease in effectiveness:[44] In any of these instances, a backup contraceptive method should be used until hormone active pills have been consistently taken for 7 consecutive days or drug-drug interactions or underlying illnesses have been discontinued or resolved.
[54] Similar to the effect of using a constant-dosage formulation and skipping the placebo weeks for three months, Seasonale gives the benefit of less frequent periods, at the potential drawback of breakthrough bleeding.
[citation needed] It is the progestin component of combined oral contraceptive pills that protects the endometrium from hyperplasia, and thus reduces a woman with PCOS's endometrial cancer risk.
[citation needed] For pelvic pain associated with endometriosis, combined oral contraceptive pills are considered a first-line medical treatment, along with NSAIDs, GnRH agonists, and aromatase inhibitors.
[4][105][120] Two large cohort studies published in 2010 both found a significant reduction in adjusted relative risk of ovarian and endometrial cancer mortality in ever-users of OCs compared with never-users.
[127] A 2016 systematic review found low quality evidence that studies of combination hormonal contraceptives showed no large difference in weight when compared with placebo or no intervention groups.
[134] In 2019, Neuroscience & Biobehavioral Reviews published a meta-analysis of 22 published and 4 unpublished studies (with 7,529 female subjects in total) that evaluated whether women expose themselves to greater health risks at different points in the menstrual cycle including by sexual activity with partners and found that subjects in the last third of the follicular phase and at ovulation (when levels of endogenous estradiol and luteinizing hormones are heightened) experienced increased sexual activity with partners as compared with the luteal phase and during menstruation.
In 2020, The Lancet Diabetes & Endocrinology published a cross-sectional study of 588 premenopausal female subjects aged 18 to 39 years from the Australian states of Queensland, New South Wales, and Victoria with regular menstrual cycles whose SHBG levels were measured by immunoassay that found that after controlling for age, body mass index, cycle stage, smoking, parity, partner status, and psychoactive medication, SHBG was inversely correlated with sexual desire.
[151] Other side effects associated with low-dose combined oral contraceptive pills are leukorrhea (increased vaginal secretions), reductions in menstrual flow, mastalgia (breast tenderness), and decrease in acne.
[medical citation needed] Excess estrogen, such as from birth control pills, appears to increase cholesterol levels in bile and decrease gallbladder movement, which can lead to gallstones.
In addition cautions are given about broad spectrum antibiotics, such as ampicillin and doxycycline, which may cause problems "by impairing the bacterial flora responsible for recycling ethinylestradiol from the large bowel" (BNF 2003).
[160][161][162][163] The traditional medicinal herb St John's Wort has also been implicated due to its upregulation of the P450 system in the liver which could increase the metabolism of ethinyl estradiol and progestin components of some combined oral contraception.
[177] In 1939, Russell Marker, a professor of organic chemistry at Pennsylvania State University, developed a method of synthesizing progesterone from plant steroid sapogenins, initially using sarsapogenin from sarsaparilla, which proved too expensive.
Unable to interest his research sponsor Parke-Davis in the commercial potential of synthesizing progesterone from Mexican yams, Marker left Penn State and in 1944 co-founded Syntex with two partners in Mexico City.
[182] In 1951, reproductive physiologist Gregory Pincus, a leader in hormone research and co-founder of the Worcester Foundation for Experimental Biology (WFEB) in Shrewsbury, Massachusetts, first met American birth control movement founder Margaret Sanger at a Manhattan dinner hosted by Abraham Stone, medical director and vice president of Planned Parenthood (PPFA), who helped Pincus obtain a small grant from PPFA to begin hormonal contraceptive research.
[183][184][185] Research started in April 1951, with reproductive physiologist Min Chueh Chang repeating and extending the 1937 experiments of Makepeace et al. that was published in 1953 and showed that injections of progesterone suppressed ovulation in rabbits.
[182] In October 1951, G. D. Searle & Company refused Pincus' request to fund his hormonal contraceptive research, but retained him as a consultant and continued to provide chemical compounds to evaluate.
In 1952, Rock induced a three-month anovulatory "pseudopregnancy" state in eighty of his infertility patients with continuous gradually increasing oral doses of an estrogen (5 to 30 mg/day diethylstilbestrol) and progesterone (50 to 300 mg/day), and within the following four months 15% of the women became pregnant.
[182][194] In October 1951, Chemist Luis Miramontes, working under the supervision of Carl Djerassi, and the direction of George Rosenkranz at Syntex in Mexico City, synthesized the first oral contraceptive, which was based on highly active progestin norethisterone.
[181][207] The first published case report of a blood clot and pulmonary embolism in a woman using Enavid (Enovid 10 mg in the US) at a dose of 20 mg/day did not appear until November 1961, four years after its approval, by which time it had been used by over one million women.
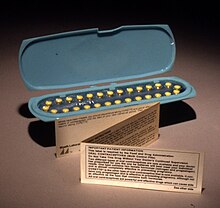
[207] Their work led to mandating the inclusion of patient package inserts with oral contraceptives to explain their possible side effects and risks to help facilitate informed consent.
[214] Pharmacists in Oregon, California, Colorado, Hawaii, Maryland, and New Mexico have authority to prescribe birth control after receiving specialized training and certification from their respective state Board of Pharmacy.
[243] The Secretary of Health, Education, and Welfare at the time, Robert Finch, announced the federal government had accepted a compromise warning statement which would accompany all sales of birth control pills.
[249] This excretion is shown to play a role in causing endocrine disruption, which affects the sexual development and reproduction of wild fish populations in segments of streams contaminated by treated sewage effluents.
[251] Several studies have suggested that reducing human population growth through increased access to contraception, including birth control pills, can be an effective strategy for climate change mitigation as well as adaptation.
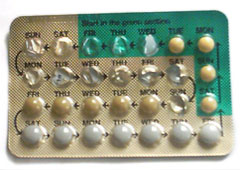
Cycle control is enhanced by the estrogen.Because combined oral contraceptives so effectively suppress ovulation and block ascent of sperm into the upper genital tract, the potential impact on endometrial receptivity to implantation is almost academic.