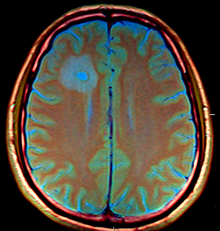
Brain abscess
[2] The famous triad of fever, headache and focal neurologic findings are highly suggestive of brain abscess.
These symptoms are caused by a combination of increased intracranial pressure due to a space-occupying lesion (headache, vomiting, confusion, coma), infection (fever, fatigue etc.)
[3] The most frequent presenting symptoms are headache, drowsiness, confusion, seizures, hemiparesis or speech difficulties together with fever with a rapidly progressive course.
An abscess in the cerebellum, for instance, may cause additional complaints as a result of brain stem compression and hydrocephalus.
[7] Bacterial abscesses rarely (if ever) arise de novo within the brain although establishing a cause can be difficult in many cases.
In cases of trauma, for example in compound skull fractures where fragments of bone are pushed into the substance of the brain, the cause of the abscess is obvious.
Other causes include: Nocardia asteroides, Mycobacterium, Fungi (e.g. Aspergillus, Candida, Cryptococcus, Mucorales, Coccidioides, Histoplasma capsulatum, Blastomyces dermatitidis, Bipolaris, Exophiala dermatitidis, Curvularia pallescens, Ochroconis gallopava, Ramichloridium mackenziei, Pseudallescheria boydii), Protozoa (e.g. Toxoplasma gondii, Entamoeba histolytica, Trypanosoma cruzi, Schistosoma, Paragonimus), and Helminths (e.g. Taenia solium).
[citation needed] The treatment includes lowering the increased intracranial pressure and starting intravenous antibiotics (and meanwhile identifying the causative organism mainly by blood culture studies).
Secondary functions of HBOT include increased stem cell production and up-regulation of VEGF which aid in the healing and recovery process.
The use of pre-operative imaging, intervention with post-operative clinical and biochemical monitoring used to manage brain abscesses today dates back to the Pennybacker system pioneered by Somerset, Kentucky-born neurosurgeon Joseph Buford Pennybacker, director of the neurosurgery department of the Radcliffe Infirmary, Oxford from 1952 to 1971.