Cerebrospinal fluid leak
[2][3] Causes of a primary CSF leak are those of trauma including from an accident or intentional injury, or arising from a medical intervention known as iatrogenic.
[5][9] A loss of CSF greater than its rate of production leads to a decreased volume inside the skull known as intracranial hypotension.
Other symptoms can include neck pain or stiffness, nausea, vomiting, dizziness, fatigue, and a metallic taste in the mouth.
[32] Other symptoms of a CSF leak include photophobia, dizziness and vertigo, gait disturbances, tinnitus, facial numbness or weakness, visual disturbances, brain fog or difficulties with concentration, neuralgia, fatigue, fluid dripping from the nose or ears,[33][23] Aural symptoms are also present in many cases of intracranial hypotension due to CSF leak; including muffled hearing, pulsatile tinnitus, hearing loss.
[34] Movement disorders are uncommon in spontaneous CSF leaks but occasionally can be one of the major components of the clinical presentation.
[35] Some cases of chronic intracranial hypotension due to CSF leak may present as personality changes, altered behaviors and impairment of executive functions, similar to behavioral-variant frontotemporal dementia as the frontal and temporal lobes are affected by downward sagging due to reduced intra-cranial pressures.
[34] An untreated CSF leak can result in coma or death as late stage findings as the brainstem herniates through the skull base or foramen magnum .
"Recent radiological and microsurgical investigations revealed that a calcified, degenerative bony microspur is often the culprit lesion in cases of intractable CSF leaks.
Arising from the level of the intervertebrate disk space, these microspurs pierce the ventral dura and produce a slit-like defect a few millimeters in length.
"[38][39] Various scientists and physicians have suggested that sCSFLs may be the result of an underlying connective tissue disorder affecting the spinal dura.
[24] Roughly 20% of patients with a sCSFL exhibit features of Marfan syndrome, including tall stature, hollowed chest (pectus excavatum), joint hypermobility and arched palate.
[45] According to this theory, dural holes and intracranial hypotension are symptoms caused by low venous pressure in the epidural space.
The increased pressure causes a rupture of the cranial dura mater, leading to a CSF leak and intracranial hypotension.
[61] Coma due to a CSF leak has been successfully treated by using blood patches and/or fibrin glue and placing the person in the Trendelenburg position.
[62] Empty sella syndrome, a bony structure that surround the pituitary gland, occurs in CSF leak patients.
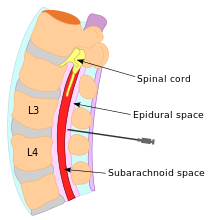
[46][63] Cerebrospinal fluid is produced by the choroid plexus in the ventricles of the brain and contained by the dura and arachnoid layers of the meninges.
[24] Lack of CSF pressure and volume can allow the brain to sag and descend through the foramen magnum (large opening) of the occipital bone, at the base of the skull.
The lower portion of the brain is believed to stretch or impact one or more cranial nerve complexes, thereby causing a variety of sensory symptoms.
[17] Diagnosis of CSF leakage can be done by various imaging techniques, chemical tests of bodily fluid discharged from a head orifice, or clinical examination.
MRI studies may show pachymeningeal enhancement (when the dura mater looks thick and inflamed), sagging of the brain, pituitary enlargement, subdural hygromas, engorgement of cerebral venous sinuses, and other abnormalities.
[69] Cerebellar tonsillar ectopia shares many of the same symptoms as CSF leak,[58] but originates either congenitally or from trauma, including whiplash strain to the dura.
[24] Contrast-enhanced brain MRI with sagittal reformats can assess for the following:[6][8] For suspected spinal CSF leaks, spine imaging can be used to guide treatment.
This is hypothesized to be due to increased permeability of dilated meningeal blood vessels and a decrease of CSF flow in the lumbar subarachnoid space.
[76][7] In addition, presence of a hyperdense paraspinal vein should be investigated in imaging as it is highly suggestive of a CSF venous fistula.
[24] Alternatively, a small compress called a pledget can be placed over the dura leak and then sealed with gel foam and fibrin glue.
[24] The use of antibiotics to prevent meningitis in those with a CSF leak due to a basilar skull fracture is of unclear benefit.
[42] Spontaneous CSF leaks have been described by notable physicians and reported in medical journals dating back to the early 1900s.
[93][94] German neurologist Georg Schaltenbrand reported in 1938 and 1953 what he termed "aliquorrhea", a condition marked by very low, unobtainable, or even negative CSF pressures.
The full clinical manifestations of intracranial hypotension and CSF leaks were described in several publications reported between the 1960s and early 1990s.
[24] The gene TGFBR2 has been implicated in several connective tissue disorders including Marfan syndrome, arterial tortuosity, and thoracic aortic aneurysm.