Breast implant
Furthermore, the women reported long-term satisfaction with their breast implant outcomes; some despite having medical complications that required surgical revision, either corrective or aesthetic.
Moreover, additional to the suicide-risk, women with breast implants also faced a trebled death-risk from alcoholism and the abuse of prescription and recreational drugs.
[23] Therefore, before agreeing to any surgery, the plastic surgeon evaluates and considers the woman's mental health to determine if breast implants can positively affect her self-esteem and sexual functioning.
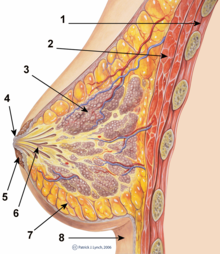
The plastic surgical emplacement of breast implant devices, either for breast reconstruction or for aesthetic purpose, presents the same health risks common to surgery, such as adverse reaction to anesthesia, hematoma (post-operative bleeding), late hematoma (post-operative bleeding after 6 months or more),[24] seroma (fluid accumulation), incision-site breakdown (wound infection).
Specific treatments for the complications of indwelling breast implants—capsular contracture and capsular rupture—are periodic MRI monitoring and physical examinations.
[28] In the 1990s, several reports reviewed the few studies evaluating any increased risk of systemic and auto-immune diseases among women with breast implants.
[29][30] However, the Institute of Medicine report pointed out that these earlier studies included too few women to conclusively evaluate the impact on these rare diseases.
The same authors also published a study on the impact of breast implant removal on breathing difficulties and found a statistically significant improvement in well-established objective measures of pulmonary function following explant surgery.
[46] In a study of his 4761 augmentation mammaplasty patients, Eisenberg reported that overfilling saline breast implants 10-13% significantly reduced the rupture-deflation rate to 1.83% at 8-years post-implantation.
[56] The first series of MRI evaluations of the silicone breast implants with thick filler-gel reported a device-rupture rate of 1 percent, or less, at the median 6-year device-age.
[25] Nonetheless, beyond the U.S., the medical establishments of other nations have not endorsed routine MRI screening, and, in its stead, proposed that such a radiologic examination be reserved for two purposes: (i) for the woman with a suspected breast implant rupture; and (ii) for the confirmation of mammographic and ultrasonic studies that indicate the presence of a ruptured breast implant.
The cause of capsular contracture is unknown, but the common incidence factors include bacterial contamination, device-shell rupture, filler leakage, and hematoma.
[65][66] The correction of capsular contracture might require an open capsulotomy (surgical release) of the collagen-fiber capsule, or the removal, and possible replacement, of the breast implant.
Common revision surgery indications include major and minor medical complications, capsular contracture, shell rupture, and device deflation.
Carefully matching the type and size of the breast implants to the patient's pectoral soft-tissue characteristics reduces the incidence of revision surgery.
The researchers found a statistically significant 22 percent increase in several diagnosed diseases, increasing to more than 60% for Sjogren's syndrome, multiple sclerosis, and sarcoidosis[31] After investigating this issue, in 2021 the U.S. FDA revised its "black box warnings" on breast implants to acknowledge the association between breast implants and systemic autoimmune, rheumatologic, and neurological symptoms to state: "Patients receiving breast implants have reported a variety of systemic symptoms, such as joint pain, muscle aches, confusion, chronic fatigue, autoimmune diseases, and others.
[77] The FDA revisited this study and additional literature several years later, reaffirming prior conclusions that platinum catalysts used in implants is likely not ionized and therefore would not represent a risk to women.
They concluded that "Breast implant-associated ALCL is a novel manifestation of site- and material-specific lymphoma originating in a specific scar location, presenting a wide array of diverse characteristics and suggesting a multifactorial cause."
[82] If women with implants present with delayed swelling or fluid collection, cytologic studies and a test for the marker CD30 are suggested.
The American Society of Plastic Surgery (ASPS) states, "CD30 is the main diagnostic test that must be performed on the seroma fluid as routine pathology or H&E staining can frequently miss the diagnosis.
"[83] Diagnosis and treatment of breast implant-associated ALCL now follows standardized guidelines established by the National Comprehensive Cancer Network.
[84] The current lifetime risk of BIA-ALCL in the U.S. is unknown, but estimates have ranged between one in 70,000 and one in 500,000 women with breast implants, according to the MD Anderson Cancer Center.
The most common reported symptom of BIA-ALCL according to the FDA was seroma, followed by breast swelling and pain, capsular contracture, and peri-implant mass or lump.
The ASPS and the Plastic Surgery Foundation (PSF) have partnered with the FDA to study this condition and in doing so created the Patient Registry and Outcomes for Breast Implants and Anaplastic Large Cell Lymphoma Etiology and Epidemiology (PROFILE).
The United States FDA strongly encourages all physicians to report cases to PROFILE in an effort to better understand the role of breast implants in ALCL and the management of this disease.
Depending upon the daily-life physical activities required of the woman, the breast augmentation patient usually resumes her normal life at 1-week post-operative.
The contemporary models of saline breast implant are manufactured with thicker, room-temperature vulcanized (RTV) shells made of a silicone elastomer.
[citation needed] The modern prosthetic breast was invented in 1961 by the American plastic surgeons Thomas Cronin and Frank Gerow, and manufactured by the Dow Corning Corporation; in due course, the first augmentation mammoplasty was performed in 1962.
[107] In the 1970s, manufacturers presented the second generation of breast implant prostheses that featured functional developments and aesthetic improvements to the technology: In the 1980s, the models of the third and of the fourth generations of breast implant devices were sequential advances in manufacturing technology, such as elastomer-coated shells that decreased gel-bleed (filler leakage), and a thicker (increased-cohesion) filler gel.
[115] The presence of radiologically opaque breast implants (either saline or silicone) might interfere with the radiographic sensitivity of the mammograph, that is, the image might not show any tumor(s) present.