Breast reduction
[1] In corrective practice, the surgical techniques and praxis for reduction mammoplasty also are applied to mastopexy (breast lift).
[2][3] The patient with macromastia presents heavy, enlarged breasts that sag and cause chronic pains to the head, neck, shoulders, and back; an oversized bust also causes secondary health problems, such as poor blood circulation, impaired breathing (inability to fill the lungs with air); chafing of the skin of the chest and the lower breast (inframammary intertrigo); brassière-strap indentations to the shoulders; and the improper fit of clothes.
In the patient affected by gigantomastia (>1,000 gm overweight per breast), the average breast-volume reduction diminished the oversized bust by three brassière cup-sizes.
[5][6][7][8][9] Afterwards, the patient's ability to comfortably perform physical activities previously impeded by oversized breasts improves emotional health (self-esteem) by reducing anxiety and lessening psychological depression.
Skin care will diminish breast crease inflammation and lessen the symptoms caused by moisture, such as irritation, chafing, infection, and bleeding.
The full, corrective outcome of the surgical re-establishment of a bodily proportionate bust becomes evident at 6-months to 1-year post-operative, during which period the reduced and lifted breast tissues settle upon and into the chest.
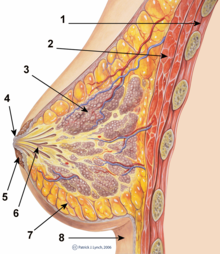
[22] The skin pedicle maintains the innervation and vascular viability of the NAC, which produces a reduced, sensitive breast with full lactational capability and function.
[citation needed] The breast reduction performed with the vertical-scar technique usually produces a well-projected bust featuring breasts with short incision scars and a NAC elevated by means of a pedicle (superior, medial, lateral) that maintains the biologic and functional viability of the NAC.
[citation needed] The breast reduction performed with the horizontal-scar technique features a horizontal incision along the inframammary fold (IMF) and a NAC pedicle.
[citation needed] The breast reduction performed with the free nipple-graft technique transposes the NAC as a tissue graft without a blood supply, without a skin and glandular pedicle.
The ideal lipectomy candidate is the patient whose low-density breasts are principally composed of adipose tissue, have a relatively elastic skin envelope, and manifest mild ptosis.
The therapeutic advantages of the liposuction-only technique are the small incision-scars required for access to the breast interior; hence, a shorter post-operative healing period for the incision scars.
[citation needed] The patient is laid supine upon the operating table so that the surgeon can later raise them to a sitting position that will allow visual comparison of the drape of the breasts, and an accurate assessment of the post-operative symmetry of the reduced and lifted bust.
Scheduled follow-up consultations ensure a satisfactory outcome to the breast reduction surgery, and facilitate the early identification and management of medical complications.
[citation needed] Limited evidence shows no significant benefit in the use of wound drains after reduction mammoplasty.
[28] The post-operative complications occurred include seroma, wound dehiscence, hematoma; partial NAC necrosis occurred in 10 per cent of the reduced breasts, but, after refinement of the Lejour technique, the study Vertical Mammaplasty: Early Complications After 250 Personal Consecutive Cases (1999) reported a reduced incidence rate of 7.0 percent in the 324 breast reductions performed in 167 patients.
[33][34] The second study by Daniel Lanzer, Breast Reduction with Liposuction (2002), about a 250-patient cohort, reported that the application of tumescent liposuction, as the sole reduction-mammoplasty procedure, yielded consistent results wherein none of the patients had loose breast-skin envelopes, irregular breast-shape, permanent loss of sensation (either glandular, dermal, or of the NAC), scars, tissue necrosis, or infection.
The patient is further informed of the possible medical complications, and is shown surgical photographic records of the average outcomes of breast-reduction surgery.
[citation needed] The measures of the bust: a liposuction mammoplasty procedure does not feature a surgical-incision plan delineated upon the patient's breasts, chest, and torso, but the measures of the bust are established in order to determine the required degree(s) of correction; thus, with the patient sitting erect, for each breast, the surgeon records the jugular-notch-to-nipple distances, the nipple-to-inframammary-fold distances, and any asymmetries.
Afterwards, the anaesthetized patient is laid supine upon the operating table, arms laterally extended (abducted), in order to fully expose the breasts.
Moreover, as required by the patient's physique, an intravenous (IV) pressure bag can be applied to hasten the infiltration; after the anaesthetic has numbed the breast, the plastic surgeon begins the lipectomy breast-reduction.
[citation needed] After the liposuction, the superficial layer of adipose fat is undermined with a blunt-tip, 3-mm cannula (which is not connected to a vacuum pump).
[citation needed] Technical note: for the reduction of very enlarged breasts, the plastic surgeon makes a supplementary incision just above the medial aspect of the inframammary fold.
Because the liposuction-only procedure featured only a few, small, surgical incisions, the patient quickly recovers their health, usually resuming daily life activities at 14 to 28 days post-operative – when the breast-molding dressings are changed; the patient also resumes their personal hygiene regimen, to include washing under a water shower.
Generally, the long-term rate of patient-satisfaction is high, provided that the indications for the liposuction-only technique are abided with proper patient selection.