Brucellosis
In the first stage of the disease, bacteremia occurs and leads to the classic triad of undulant fevers, sweating (often with a characteristic foul, moldy smell sometimes likened to wet hay), and migratory arthralgia and myalgia (joint and muscle pain).
The focalizations of brucellosis occur usually in bones and joints, and osteomyelitis or spondylodiscitis of the lumbar spine accompanied by sacroiliitis is very characteristic of this disease.
The consequences of Brucella infection are highly variable and may include arthritis, spondylitis, thrombocytopenia, meningitis, uveitis, optic neuritis, endocarditis, and various neurological disorders collectively known as neurobrucellosis.
Brucellosis induces inconstant fevers, miscarriage, sweating, weakness, anemia, headaches, depression, and muscular and bodily pain.
[citation needed] Overall findings support that brucellosis poses an occupational risk to goat farmers with specific areas of concern including weak awareness of disease transmission to humans and lack of knowledge on specific safe farm practices such as quarantine practices.
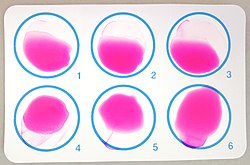
Identification of specific antibodies against bacterial lipopolysaccharide and other antigens can be detected by the standard agglutination test (SAT), rose Bengal, 2-mercaptoethanol (2-ME), antihuman globulin (Coombs') and indirect enzyme-linked immunosorbent assay (ELISA).
[citation needed] Due to the similarity of the O polysaccharide of Brucella to that of various other Gram-negative bacteria (e.g. Francisella tularensis, Escherichia coli, Salmonella urbana, Yersinia enterocolitica, Vibrio cholerae, and Stenotrophomonas maltophilia), the appearance of cross-reactions of class M immunoglobulins may occur.
False-negative SAT may be caused by the presence of blocking antibodies (the prozone phenomenon) in the α2-globulin (IgA) and in the α-globulin (IgG) fractions.
[citation needed] Dipstick assays are new and promising, based on the binding of Brucella IgM antibodies, and are simple, accurate, and rapid.
[16] Unfortunately, these are not standardized for routine use, and some centres have reported persistent PCR positivity after clinically successful treatment, fuelling the controversy about the existence of prolonged chronic brucellosis.
[citation needed] Other laboratory findings include normal peripheral white cell count, and occasional leucopenia with relative lymphocytosis.
Changing traditional food habits of eating raw meat, liver, or bone marrow is necessary, but difficult to implement.
[citation needed] Exposure of diagnostic laboratory personnel to Brucella organisms remains a problem in both endemic settings and when brucellosis is unknowingly imported by a patient.
[30][31] According to Georgios Pappas, an infectious-disease specialist and author of a report published in the journal Clinical Infectious Diseases,[32] the result was “possibly the largest laboratory accident in the history of infectious diseases.” According to Pappas, out of nearly 70,000 people tested, more than 10,000 were seropositive, citing figures compiled by the provincial health authorities in Lanzhou’s Gansu province.
Pappas also states that Chinese documents show that more than 3,000 people living near the plant applied for compensation, an indication of at least a mild illness.
In the United States, veterinarians are required [citation needed] to vaccinate all young stock, to further reduce the chance of zoonotic transmission.
[46] Maltese scientist and archaeologist Themistocles Zammit identified unpasteurized goat milk as the major etiologic factor of undulant fever in June 1905.
[47] In the late 1910s, American bacteriologist Alice C. Evans was studying the Bang bacillus and gradually realized that it was virtually indistinguishable from the Bruce coccus.
[48] The Bang bacillus was already known to be enzootic in American dairy cattle, which showed itself in the regularity with which herds experienced contagious abortion.
[48] Having made the discovery that the bacteria were certainly nearly identical and perhaps totally so, Evans then wondered why Malta fever was not widely diagnosed or reported in the United States.
[48] She began to wonder whether many cases of vaguely defined febrile illnesses were in fact caused by the drinking of raw (unpasteurized) milk.
This advance in bacteriological science sparked extensive changes in the American dairy industry to improve food safety.
[citation needed] In the decades after Evans's work, this genus, which received the name Brucella in honor of Bruce, was found to contain several species with varying virulence.
In the late 19th century, its symptoms were described in more detail by M. Louis Hughes, a Surgeon-Captain of the Royal Army Medical Corps stationed in Malta who isolated brucella organisms from a patient with meningo-encephalitis.
The stability of M114 in storage was too low to allow for storing it at forward air bases, and the logistical requirements to neutralize a target were far higher than originally planned.
[55] The most common clinical signs of cattle infected with B. abortus are high incidences of abortions, arthritic joints, and retained placenta.
The bacteria in dogs normally infect the genitals and lymphatic system, but can also spread to the eyes, kidneys, and intervertebral discs.
The recent transmission of brucellosis from elk back to cattle in Idaho and Wyoming illustrates how the area, as the last remaining reservoir in the United States, may adversely affect the livestock industry.
[58] Hunters may be at additional risk for exposure to brucellosis due to increased contact with susceptible wildlife, including predators that may have fed on infected prey.
[63] Hunters can limit exposure while cleaning game through the use of precautionary barriers, including gloves and masks, and by washing tools rigorously after use.