Cardiac output
For a healthy individual weighing 70 kg, the cardiac output at rest averages about 5 L/min; assuming a heart rate of 70 beats/min, the stroke volume would be approximately 70 mL.
Regular aerobic exercise can induce physiological adaptations such as improved stroke volume and myocardial efficiency that increase cardiac output.
The function of the heart is to drive blood through the circulatory system in a cycle that delivers oxygen, nutrients and chemicals to the body's cells and removes cellular waste.
Because it pumps out whatever blood comes back into it from the venous system, the quantity of blood returning to the heart effectively determines the quantity of blood the heart pumps out – its cardiac output, Q. Cardiac output is classically defined alongside stroke volume (SV) and the heart rate (HR) as:[citation needed] In standardizing what CO values are considered to be within normal range independent of the size of the subject's body, the accepted convention is to further index equation (1) using body surface area (BSA), giving rise to the Cardiac index (CI).
[9] It is said to require extensive training and skill, but the exact steps needed to achieve clinically adequate precision have never been disclosed.
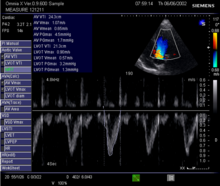
2D measurement of the aortic valve diameter is one source of noise; others are beat-to-beat variation in stroke volume and subtle differences in probe position.
Real-time, automatic tracing of the Doppler flow profile allows beat-to-beat right-sided and left-sided Q measurements, simplifying operation and reducing the time of acquisition compared to conventional echocardiography.
This method has good validation, is widely used for fluid management during surgery with evidence for improved patient outcome,[18][19][20][21][22][23][24][25] and has been recommended by the UK's National Institute for Health and Clinical Excellence (NICE).
[citation needed] In 1967, the Czech physiologist Jan Peňáz invented and patented the volume clamp method of measuring continuous blood pressure.
These methods include the use of modulated infrared light in the optical system inside the sensor, the lightweight, easy-to-wrap finger cuff with velcro fixation, a new pneumatic proportional control valve principle, and a set point strategy for the determining and tracking the correct volume at which to clamp the finger arteries—the Physiocal system.
This innovative brachial pressure waveform reconstruction method was first implemented in the Finometer, the successor of Finapres that BMI-TNO introduced to the market in 2000.
According to comparisons of non-invasive peripheral vascular monitors, modest clinical utility is restricted to patients with normal and invariant circulation.
Changes in vascular function, the position of the catheter tip or damping of the pressure waveform signal will affect the accuracy of the readings.
[citation needed] PiCCO (PULSION Medical Systems AG, Munich, Germany) and PulseCO (LiDCO Ltd, London, England) generate continuous Q by analysing the arterial PP waveform.
[30] Calibration events are limited in frequency because they involve the injection of lithium chloride and can be subject to errors in the presence of certain muscle relaxants.
The device uses an algorithm based on the Frank–Starling law of the heart, which states pulse pressure (PP) is proportional to stroke volume (SV).
The algorithm calculates the product of the standard deviation of the arterial pressure (AP) wave over a sampled period of 20 seconds and a vascular tone factor (Khi, or χ) to generate stroke volume.
A physiologic optimization program based on haemodynamic principles that incorporates the data pairs SV and SVV has been published.
Unlike FloTrac, neither constant values of impedance from external calibration, nor form pre-estimated in vivo or in vitro data, are needed.
[38][39] Generally monitored haemodynamic values, fluid responsiveness parameters and an exclusive reference are provided by PRAM: Cardiac Cycle Efficiency (CCE).
The ratio between heart performance and consumed energy, represented as CCE "stress index", can be of paramount importance in understanding the patient's present and future courses.
[53] It was extensively used to measure flow and volumes with extracorporeal circuit conditions, such as ECMO[54][55] and Haemodialysis,[56][57] leading more than 150 peer reviewed publications.
[citation needed] UD requires the establishment of an extracorporeal circulation through its unique AV loop with two pre-existing arterial and central venous lines in ICU patients.
The underlying model differs between the two methods; Electrical cardiometry attributes the steep increase of TEB beat-to-beat to the change in orientation of red blood cells.
Electrical cardiometry monitors have shown promise in postoperative cardiac surgical patients, in both haemodynamically stable and unstable cases.
[60] Velocity-encoded phase contrast Magnetic resonance imaging (MRI)[61] is the most accurate technique for measuring flow in large vessels in mammals.
[65] While MRI is an important research tool for accurately measuring Q, it is currently not clinically used for haemodynamic monitoring in emergency or intensive care settings.
The determinants of SV during the cardiac cycle are the contractility of the heart muscle, the degree of preload of myocardial distention prior to shortening and the afterload during ejection.
Other variations use inert gases as tracers and measure the change in inspired and expired gas concentrations to calculate Q (Innocor, Innovision A/S, Denmark).
[6][7][8] This clinical ineffectiveness may relate to its poor accuracy and sensitivity, which have been demonstrated by comparison with flow probes across a sixfold range of Q values.