Cervical effacement
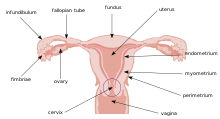
This process occurs during labor to prepare the cervix for dilation to allow the fetus to pass through the vagina.
While this is a normal, physiological process that occurs at the later end of pregnancy, it can also be induced through medications and procedures.
[3] Toward the end of pregnancy, a series of hormone-mediated biochemical process takes place to degrade the collagen and fiber network to cause the cervix to ripen during labor.
[4] Current efforts to induce labor include pharmacologic, non-pharmacologic, mechanical and surgical methods.
Due to a variety of reasons, such as cost and patient preference, the capacity to undergo outpatient cervical ripening is being explored.
Further Information: Signaling Pathways Regulating Human Cervical Ripening in Preterm and Term Delivery[6]Histologically, the cervix undergoes significant changes towards the end of gestation, allowing the ripening of cervix for the passage of birth delivery.
[7] Third, due to the nature of the cervical effacement process, enzymes and other mediators that regulate allergic and inflammatory responses are also involved.
[8] Histamine, one of the allergenic mediators released by mast cells, has shown to have causative relationship with cervical smooth muscle contractility.
The modified scoring method takes into consideration only 3 parameters: dilation, effacement, and fetal station.
[10] Given that cervical effacement is measured as a percentage, this method requires a consensus on a standard uneffaced cervix length.
This requirement presents itself as an opportunity for error, miscommunication and inappropriate care in the process of assessing cervical effacement.
Integrating the metric system of measurement of the cervix may reduce and eliminate the risk of error and assumptions on cervical length.
[16] The risk of uterine hyperstimulation as it relates to labor induction is higher with dinoprostone and vaginally administered misoprostol than it is with oxytocin and mechanical methods.
As oxytocin is one of the methods used for cervical ripening, the Committee on Obstetric Practice at the American College of Obstetricians and Gynecologists conducted a review of existing research regarding this link, and concluded that there was insufficient evidence of a causal link between cervical effacement via oxytocin and autism/ASD.
[17] Inpatient and outpatient cervical ripening done via vaginally administered dinoprostone or balloon catheters in low risk pregnancies do not have different rates of caesarean section.
This is to imitate the pressure of a fetal head that would be pressing on the cervix during labor, which in turn speeds up the process.
According to a study conducted in Japan from 2012-2014, the rate of delivery at term seemed to be equivalent between the group that used balloon catheter and that of the hygroscopic dilator.
The reason for the surgical procedure could either be for cervical effacement or to look at fetal status as a device can be inserted into the amniotic sac for monitoring.
Membrane sweeping may rupture the amniotic sac for 1 out of 10 women who get this procedure done, which will then lead for the need to formally induce labor within 24 hours.